Therapeutic patient education as the basis for diabetes long-term follow-up
Author:
Prof. Dr. med. Zoltan Pataky
Unit of therapeutic patient education
Geneva University Hospital
Faculty Diabetes Centre
Faculty of Medicine
University of Geneva
Email: zoltan.pataky@hcuge.ch
Sie sind bereits registriert?
Loggen Sie sich mit Ihrem Universimed-Benutzerkonto ein:
Sie sind noch nicht registriert?
Registrieren Sie sich jetzt kostenlos auf universimed.com und erhalten Sie Zugang zu allen Artikeln, bewerten Sie Inhalte und speichern Sie interessante Beiträge in Ihrem persönlichen Bereich
zum späteren Lesen. Ihre Registrierung ist für alle Unversimed-Portale gültig. (inkl. allgemeineplus.at & med-Diplom.at)
Diabetes treatment and management depends on a multitude of parameters, both medication-related and patients’ lifestyle-related. Diabetologists do not consider enough the hidden facets of diabetes having an important and extraordinary role in glucose homeostasis regulation. Health care providers and particularly doctors are often problem-solving oriented, having no training in long-term follow-up of chronic diseases. Diabetes needs to be understood as a chronic and complex metabolic dysregulation to which only the patient could have the key how to restore the equilibrium. For that, this patient needs understanding and positive attitudes of his doctor who unfortunately misses training in therapeutic patient education.
Keypoints
-
Diabetes is a chronic disease which treatment should consider, among others, patient’s psychosocial situation, emotions and sleep. The medication, diet and physical activity are not the only parameters impacting on intermediary metabolism.
-
The person living with diabetes is above all a human being. Classic biomedical approach with the doctor acting as a mechanic (problem solving) is no longer enough, a biopsychosocial approach is needed.
-
Diabetologists’ therapeutic approach should go beyond the classic diabetes treatment algorithms.
-
Health care providers must be trained in therapeutic patient education so that they can establish a therapeutic relationship between caregiver and patient, a conducive climate to patient education, in which the patient is considered the care partner.
The complexity of diabetes and the hidden facets of chronic diseases
The hormonal regulation of glycemic control is complex and depends on a multitude of biological parameters on one hand, and essentially on many factors linked to the patient’s lifestyle on the other hand. These factors, which are specific to every person living with diabetes, include not only the diet-related issues and the daily physical activity, but also the psychosocial situation, emotions and sleep, when all of them influence eating behavior and carbohydrate metabolism.
In fact, the hormonal regulation is closely linked to stress and emotions, which play an important role in regulating intermediary metabolism. Unfortunately, these patient-related factors are often underestimated by health care professionals (HCPs) in the long-term follow-up.
Blood sugar, as reflected by the self-monitoring or the easy-to-measure HbA1c, as well as the micro- and macro-vascular complications of diabetes, which are easy to detect using available diagnostic methods, represent only the tip of the iceberg related to diabetes. In other words, these medical aspects are easy to put in evidence and they require expertise that is well trained at medical schools and during the residency programs for future diabetologists.
However, any HCP taking care of people with chronic diseases such as diabetes must consider the psychosocial aspects of his patient’s life and cannot be satisfied with the biomedical aspect alone to treat any patient.
In fact, every person with diabetes is unique, with their own life, their own personal experiences and their own emotions they live with daily. The diagnosis of diabetes is often difficult to accept for the patient, and is often experienced as an injustice, with feelings of frustration (for example in relation to our dietary “advice” we usually do), loneliness, fear, and stress. Patients could feel judged by their doctor or other HCPs, afraid of disappointing them, and so on. All because the people affected by diabetes have to “carry” it daily, all their lives.
In fact, the disease is present regardless of what the patients do, where and with whom they are. This same patient does not have only his diabetes in his life and cannot deal only with the disease permanently. Doctors, however, act as if the patient has nothing else to do but to deal with the disease, and they expect their patients to follow their advice to the letter.
After diagnosing diabetes, the doctor proposes a treatment based on what he has learned: he follows guidelines and algorithms. Obviously, this is an important step that the doctor must respect. On the other hand, and regardless of the treatment (oral antidiabetics, insulin, GLP-1 agonists, or different treatment combinations), its effectiveness will depend mainly on all the parameters that the doctor does not control. And this is often where the doctor tends to underestimate the person-related aspects, linked to the individual, his origins, his culture, his private and professional life, his worries, his stress, his daily experiences. These are the hidden facets of chronic diseases, yet they play a crucial role in the homeostatic balance of which blood sugar is an integral part.
This is where the doctor lacks the competence to integrate the person into the therapeutic process. Sad to say, this same doctor thinks he has done everything possible to treat his patient well.
For long-term treatment of any patient suffering from this chronic disease, it is mandatory to consider these hidden facets, this biopsychosocial dimension of diabetes.
We think we are on the right way, we have learned it: is it enough?
For many diabetologists, the evidence-based treatment of diabetes consists in prescribing the glucose lowering medication according to the HbA1c value, the glucose self-monitoring and regarding the presence of complications or other risk factors. Some of us, doctors, are aware that this approach may not be enough because after some period of treatment, the biomedical results are not exactly corresponding to our expectations (e.g., permanently high HbA1c).
What is happening in these clinical situations for some of the HCPs? The patient is not compliant, he is not listening to the doctor’s advice and recommendations. For the doctor, he is applying what he had learned during his medical studies and residency years, he is just following algorithms and guidelines. Where is the real problem?
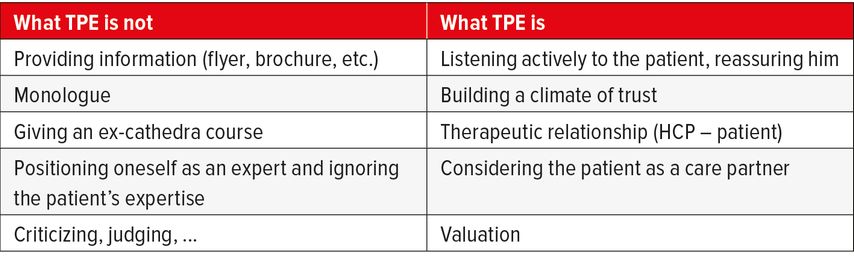
Many HCPs say that they provide therapeutic patient education (TPE) in their daily practice. For most of them, they “educate” their patients. Mostly, HCPs consider TPE as to giving information to the patient, explaining how to perform glucose self-monitoring, how to fit a continuous glucose monitor sensor or how to make injections. In hospital, doctors often refer patients to nurses to “perform” TPE. However, is this correct and enough to treat and follow-up a patient with a life-long disease such as diabetes? Table 1 highlights some basic differences concerning TPE.
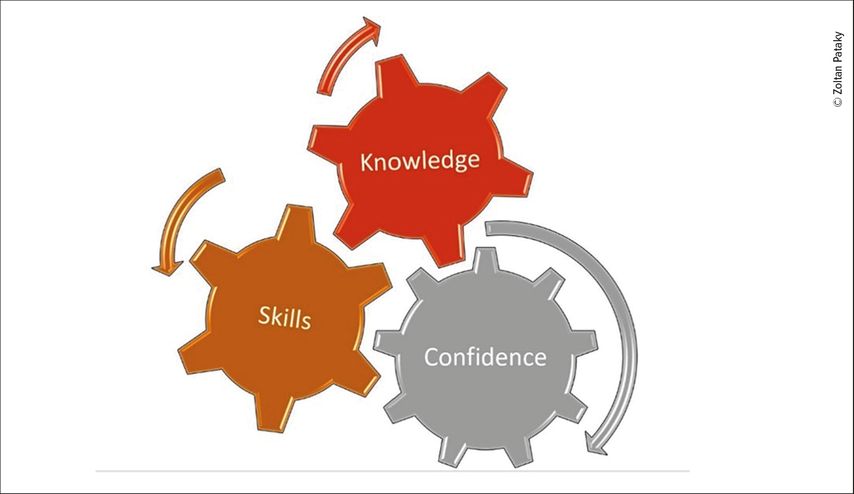
Knowledge and skills are not in themselves enough to support a patient to self-manage his/her condition. The patient also needs to feel to be confident to self-manage his/her condition. Together, knowledge, skills and confidence can lead to a change in behavior and an ability to self-manage their condition and its consequences. These three competencies form a patient competency framework (Fig. 1) which underpins the design of self-management support and therapeutic patient education interventions.
The doctor’s professional identity
The doctor or any other HCP is first and foremost an expert who has the expertise in relation to his medical specialty. But can this same HCP ignore the expertise and experiences of his/her patient, who lives with diabetes daily and whom no-one else knows better then he himself/she herself?
It is mandatory to remain focused on the patient as an individual, rather than constantly focusing on the disease and the laboratory findings. Unfortunately, doctors see the patient as a sum of organs, while each specialist puts his own spin on things, related to his field of interest which is related to his medical specialty, and forgetting the essential point: the person with diabetes is first and foremost a human being. The doctor must essentially rely on the patient’s story, on his own difficulties, before even talking about the disease and its treatment. He must draw on the patient’s experience and expertise and empower the patient, motivate him/her to accept and take care of the disease in the long term.
Unfortunately, the nature of the medical identity, related to medical studies, means that doctors are “stripped” of their power, which consists of holding knowledge in the spirit of the power to treat and heal. Consequently, a doctor who is firmly attached to his image as an all-powerful expert is counterproductive for the patient and leads to postures and counter-attitudes that are the opposite of what a true therapeutic relationship with a patient requires.
The fundamentals of therapeutic patient education
As mentioned above and illustrated in Table 1 and Figure 1, TPE does not simply mean giving information to the patient. TPE starts with the HCP’s spontaneous attitude, and it is only possible if the doctor’s therapeutic approach goes beyond the classic diabetes treatment algorithms. TPE begins with the doctor adopting the posture needed to approach the person in front of him. The doctor should establish a climate of trust between himself and his patient. In this therapeutic relationship based on mutual respect and trust, it is then possible to discuss subjects that are difficult to access if the patient does not feel that he is being listened to and understood by his therapist. It is very important to adapt the language used to patients, who do not always understand what the doctor is telling them, and rightly so.
The HCP should ensure that he has understood what the patient is saying (reformulation) and, above all, give the patient enough space to express his experiences, fears, worries, or simply questions. Once the HCP has grasped the real difficulties of the person in front of him, he should be able to use this information wisely.
The therapeutic objective follows on from the educational diagnosis that the doctor should be able to formulate with the patient.
This management of the patient as a whole and the “decentralization” from the classical disease-centered approach, requires training.
Do we all have a chance to be trained to TPE? It is sad to note that in 2023, most of us are only learning about the biomedical aspects of diabetes treatment, while we continue to say that we are practicing TPE on a daily basis and we are no more disease-centered.
For an HCP, recognition of the expertise of patients who live with their diseases is just as important as knowledge of the latest evidence-based treatments.
The diabetologist sees his patient during a 20–30-minute consultation to check, among others, the HbA1c, which reflects the patient’s diabetes control over the last 3 months. This consultation time corresponds to 0,0002% over a 3-month period. The rest of the time, the patient is on his own, without his doctor. That is why it is mandatory to take into account the patient’s expertise, to listen carefully (active listening), and to rephrase what they are saying to ensure that they understand what they are telling their doctor.
But how do we “process” all the important information that patients give us? Doctors are not trained in comprehension interview to correctly interpret the patient’s story and to integrate his said experience into therapeutic process and shared decision making. As mentioned above, to give information (knowledge) to the patient is far from TPE process.
Therapeutic patient education was developed to help HCP’s treat people suffering from diabetes
TPE comes as an answer to the many questions patients ask, and for which they do not receive any answers because diabetologists/doctors in general maintain their “formatted” posture during their studies, a classic biomedical approach.
The principles of TPE have developed from evidence-based concepts and models from a number of disciplines, including behavioral sciences, health systems, and adult education.
The foundations of TPE were developed in the 1970s in Europe, in parallel with the USA. Leona Miller published an article in the New England Journal of Medicine in 19721 and showed that with an approach that went beyond conventional biomedical treatment, diabetic patients managed to reduce the length of hospital stay from 5,4 to 1,7days/year/patient. The incidence of diabetic comas was also reduced by two-thirds.1
In Europe, and more particularly in Switzerland, Jean-Philippe Assal, internist, set up a diabetes treatment and teaching unit at Geneva University Hospitals in 1975. It was a pioneering unit that succeeded in integrating a bio-psycho-social approach into diabetology. By integrating a psychologist and a specialist of adult pedagogy into a multidisciplinary team composed of doctors, nurses and dieticians at the outset, the doctors were finally able to better highlight the real need to integrate this dimension other than purely medical into the follow-up of patients suffering from a chronic disease such as diabetes.
TPE was subsequently defined by the WHO in 1983,2 following an initiative by Jean-Philippe Assal, who brought together international experts and made recommendations to healthcare providers. Since then, on the WHO’s recommendation, TPE should be an integral part of the management of any diabetic patient (like any patient suffering from any chronic disease). Unfortunately, TPE continues not to be integrated into these treatments and often goes unrecognized by diabetologists and sometimes even by heads of specialized diabetes centers. The main argument put forward by doctors who continue to ignore the larger bio-psycho-social management of diabetes, based on TPE, is that it is not effective.
The effectiveness of TPE
High-quality evidence has consistently shown that TPE significantly improves knowledge, glycemic levels, and clinical and psychological outcomes, reduces hospital admissions and all-cause mortality and is cost-effective.e.g. 3–6
Very recently, in a systematic review and meta-analysis, we demonstrated that patients suffering from diabetes and obesity who benefited from structured TPE interventions showed significant improvements not only in glycemic control (HbA1c) and weight loss (BMI) but also in psychosocial functioning and quality of life, compared with patients who did not benefit from a TPE approach.7 Moreover, these results were observed for all the chronic diseases studied, without exception.8
The place of TPE in therapeutic recommendations for the treatment of diabetes
All guidelines consider diabetes patient education as one of the cornerstones of diabetes management. As an example, and according to American Diabetes Association (ADA),9 to ADA and European Association for the Study of Diabetes (EASD) consensus report,10 all people with diabetes should participate in diabetes self-management education and support to facilitate the knowledge, decision-making, and skills mastery for diabetes self-care (level of evidence and grade of recommendation category A). The diabetes algorithm of the American Association of Clinical Endocrinology 2023 update emphasizes lifestyle modification related to diabetes and treatment of overweight and obesity as key pillars in the management of prediabetes and diabetes mellitus.11 In Switzerland, the Swiss Diabetes and Endocrine Society is defining the lifestyle intervention as the first-line treatment of prediabetes and diabetes at all ages.12
Conclusions
Any health professional who takes care of patients with diabetes should benefit from training in the principles of diabetes self-management and support as well as TPE. There is strong evidence that TPE should be an integral part of any chronic disease management. Diabetes is a scholar example of such a disease.
Embedding an understanding of TPE early on in a professional’s training curricula can lead to long-term benefits, such as more person-centered care and health care providers who focus on empowering patients and caregivers in self-management, and can lower the burden on the health sector.
Literature:
1 Miller LV, Goldstein J: More efficient care of diabetic patients in a county-hospital setting. N Engl J Med 1972; 286: 1388-91 2 World Health Organization. Regional Office for Europe: Therapeutic patient education: continuing education programmes for health care providers in the field of prevention of chronic diseases: report of a WHO working group. World Health Organization 1998; Regional Office for Europe. https://apps.who.int/iris/handle/10665/108151 3 American Diabetes Association Professional Practice Committee et al.: 5. Facilitating behavior change and well-being to improve health outcomes: Standards of Medical Care in Diabetes – 2022. Diabetes Care 2022; 45 (Suppl 1): 60-82 4 Odgers-Jewell K et al.: Effectiveness of group-based self-management education for individuals with type 2 diabetes: a systematic review with meta-analyses and meta-regression. Diabet Med 2017; 34: 1027-39 5 He X et al.: Diabetes self-management education reduces risk of all-cause mortality in type 2 diabetes patients: a systematic review and meta-analysis. Endocrine 2017; 55: 712-31 6 Chatterjee S et al.: Diabetes structured self-management education programmes: a narrative review and current innovations. Lancet Diabetes Endocrinol 2018, 6: 130-42 7 Correia JC et al.: Effectiveness of therapeutic patient education interventions in obesity and diabetes: a systematic review and meta-analysis of randomized controlled trials. Nutrients 2022; 14: 3807 8 Correia JC et al.: Effectiveness of therapeutic patient education interventions for chronic diseases: A systematic review and meta-analyses of randomized controlled trials. Front med 2023; doi: 10.3389/fmed.2022.996528 9 ElSayed NA et al.: Facilitating positive health behaviors and well-being to improve health outcomes: standards of care in diabetes—2023. Diabetes Care 2023; 46 (Suppl. 1): 68-96 10 Davies MJ et al.: Management of hyperglycemia in type 2 diabetes, 2022. A consensus report by the American Diabetes Association and the European Association for the Study of Diabetes, Diabetologia 2022; 65: 1925-66 11 Samson SL et al.: American Association of Clinical Endocrinology Consensus Statement: Comprehensive type 2 diabetes management algorithm – 2023 update. Endocrine Practice 2023; 29: 305-40 12 Gastaldi G et al.: Swiss recommendations of the Society for Endocrinology and Diabetes (SGED/SSED) for the treatment of type 2 diabetes mellitus (2023). Swiss Med Wkly 2023; 153: 40060
Das könnte Sie auch interessieren:
Tachycardie supraventriculaire
Les tachycardies paroxystiques supraventriculaires régulières apparaissent généralement chez des patients sans cardiopathie structurelle. Dans cet article, nous discutons de l’importance ...
Risques du tabagisme pour la santé – sevrage tabagique
«Un fumeur avide qui lit et relit l’importance des risques du tabagisme pour sa santé cesse dans la plupart des cas ... de lire», avait déclaré Winston Churchill. «Le tabac est le seul ...
Diabète et foie
De nombreuses personnes souffrant d’obésité ou de diabète de type 2 (DT2) développent au cours de leur vie une maladie hépatique stéatosique associée à un dysfonctionnement métabolique ( ...