An expanding concept: the orthoplastic approach
Authors:
Dr. med. Anita Hasler
Prof. Dr. med. Jan Plock
Klinik für Plastische Chirurgie und Handchirurgie Kantonsspital Aarau
E-Mail: anita.hasler@ksa.ch
Sie sind bereits registriert?
Loggen Sie sich mit Ihrem Universimed-Benutzerkonto ein:
Sie sind noch nicht registriert?
Registrieren Sie sich jetzt kostenlos auf universimed.com und erhalten Sie Zugang zu allen Artikeln, bewerten Sie Inhalte und speichern Sie interessante Beiträge in Ihrem persönlichen Bereich
zum späteren Lesen. Ihre Registrierung ist für alle Unversimed-Portale gültig. (inkl. allgemeineplus.at & med-Diplom.at)
Orthoplastic surgery is a multidisciplinary service that provides the best possible care for patients with complex limb conditions. This approach is gaining popularity worldwide as the benefits of this collaboration between orthopedic and plastic surgeons are substantiated by latest research. The following article reviews the history and current concepts of orthoplastic surgery and illustrates the diversity, complexity and beneficial outcome in three cases.
Keypoints
-
Orthoplastic surgery is an evidence-based approach improving outcomes for patients with complex limb conditions.
-
Interdisciplinary collaboration should begin in the emergency department and continue throughout follow-up.
-
Structured, regular meetings can provide a platform for this exchange between disciplines.
Definition Orthoplastic Approach
The orthoplastic approach, described in 1993 by Scott Levin,1 incorporates immediate multidisciplinary collaboration for the management of traumatic lower extremity injuries. For high-energy trauma, orthopedic surgeons provide expertise for osseous fixation and frequently plastic surgeons are consulted to optimize conditions for soft-tissue reconstruction relying heavily on microvascular techniques. The orthoplastic approach has been applied for patients with all sort of complex limb condition caused by trauma, infection or tumor in the meantime.
History
Evidence for one of the earlies collaborations between orthopaedic and plastic surgery has been provided by W. Arbuthnot Lane, an orthopaedic surgeon, who wrote the preface for Sir Harold Gillies’ plastic surgery textbook in 1919.2
Further development of the orthoplastic approach has been closely linked to the beginning of the vascular surgery era. 1902 Alexis Carrel descripted the first end-to-end vascular anastomosis3 and later in 1960 Jacobson and Suarez performed a microvascular anastomosis using an operative microscope.4 Advancements in microsurgical instrumentation, sutures, and needles led to the evolution of modern microsurgery.5 From this era until today, innovations have continued including widespread use of muscle, fasciocutaneous, perforator, and vascularized bone flaps. Combined, these microsurgical advancements have become the pillars of orthoplastic surgery.2
Advantages Orthoplastic Approach
Several studies have investigated the benefit of an orthoplastic approach in different patient groups (Tab. I). The search term «orthoplastic» leads to over 700 articles at pubmed, with 140 articles using this search term alone since 2020.
Open fractures
The primary goal for open fractures has been represented by initial skeletal stabilization within 24 hours and staged definitive soft tissue coverage within 72 hours of the initial injury.9 These standards were based on evidence for better outcomes with early definitive treatment.10,11,12 Fix and flap was introduced as a concept by Gopal in 2000.11 The authors presented a simultaneous protocol that included early soft tissue coverage with a muscle flap during bone surgery by a combined orthopedic and plastic surgery service. In their retrospective study of 84 patients, who had sustained a severe open fracture (Gustilo IIIb or IIIc) of the tibia, the authors demonstrated that delayed wound coverage (>72 hours) was associated with a higher complication rate in comparison to an early approach including simultaneous bone fixation and flap surgery. Patients with late soft tissue coverage (>72 hours to coverage) experienced 30% deep infections, whereas only 3% deep infections were detected in the immediate flap group (<24 hours).
In 2021, a systematic review by Klifto et al. compared 1663 patients managed by joint orthoplastic service to 692 patients managed in a traditional non-orthoplastic approach for traumatic lower extremity injuries.6 The authors provided evidence that an orthoplastic approach decreased the time to bone fixation, reduced the use of negative pressure wound therapy (NPWT) as well as the risk of wound infections and osteomyelitis, respectively. In the same year, Hoyt et al. demonstrated similar advantageous outcome for combat-related extremity trauma treated with an orthoplastic approach. In their study of a total of 307 patients, the collaborative orthoplastic team approach resulted in decreased flap failures (odds ratio 0,4 [95% confidence interval 0,2 to 0,9]; p=0,02).7 Also in the treatment of severe open tibial fractures, the orthoplastic approach was associated with improved clinical outcome, such as quicker time to bone union, more durable soft tissue coverage, less pain, better function, and fewer complications than the exclusively orthopaedic approach.8
With a special weekly orthoplastic surgical list, the time to final soft tissue coverage was significantly reduced from 112,8 to 65,4 hours (p=0,019) for all Gustilo-Anderson grades.13 For Gustilo-Anderson grades IIIb and IIIb, the study was able to show that the introduction of the orthoplastic surgical list significantly reduced the time to soft tissue coverage (173,6h vs. 88,1h, p=0,009), and significantly increased the 72-hour soft tissue coverage goal from 20,0% to 53,6% (p=0,019).
Limb salvage or amputation
In addition to the evidence summarized above for improved overall outcomes in open fractures with an orthopedic approach, interdisciplinarity may also facilitate decision making in favor of limb preservation or amputation. Because of the lack of indicators for salvageable limbs, the decision to reconstruct or amputate must often be made based on the judgment of a multidisciplinary orthoplastic team.14,15,16 If amputation is to be performed, the orthoplastic team should attempt to preserve sufficient length and sensibility for effective prosthetic fitting and utilize the principles of spare-part surgery, fillet flaps, island pedicle flaps, and free flaps as needed.17 These different considerations of an orthoplastic approach are illustrated in case 3 (see Figure 3).
Sarcoma surgery
Progress in microsurgery has helped not only to improve limb salvage rates, but also to create wider margins without altering oncologic goals of curative resection. Although limb salvage is only a secondary goal of tumor surgery, progression in microsurgery and reconstructive surgery lead to potential reconstructice benefits without impacting tumor safety and complication rate.18 It is well known that microsurgical reconstruction after sarcoma surgery is reliable and safe19,20 but due to the rarity of those tumors, there are no comparative studies for the use of an orthoplastic approach in the literature. Götzl et al. found in a retrospective analysis of 290 patients with soft tissue sarcoma no significant differences in complication rates when a free flap was performed compared to primary wound closure, but the local recurrence risk was over two times higher with primary wound closure than with flaps at 10 year follow-up.21
Orthoplastic service at the Cantonal Hospital Aarau (KSA)
In order to implement an orthoplastic approach at the Cantonal Hospital Aarau, close cooperation between orthopedic surgeons and plastic surgerons for the benefit of the patients has been established. Mangled extremities have been evaluated in a joint approach primarily to define the treatment plan. Besides cooperation in the emergency department, an interdisciplinary musculoskeletal infectious disease colloquium (IMSIK) has facilitated evaluation of patients in a routine weekly meeting. This meeting was created through the initiative and commitment of the Traumatology/Orthopedics Service and Infectiology at the KSA.
The following three clinical cases should highlight the major and critical key points as well as illustrate the diversity in orthoplastic cases. All cases were operated within 4 months between December 2021 and March 2022 at the Cantonal Hospital Aarau. These cases were selected to illustrate potential challenges in collaboration and the range from soft tissue coverage over functional reconstruction to 3-D guided reconstructive surgery and sparing parts reconstruction.
Case I:
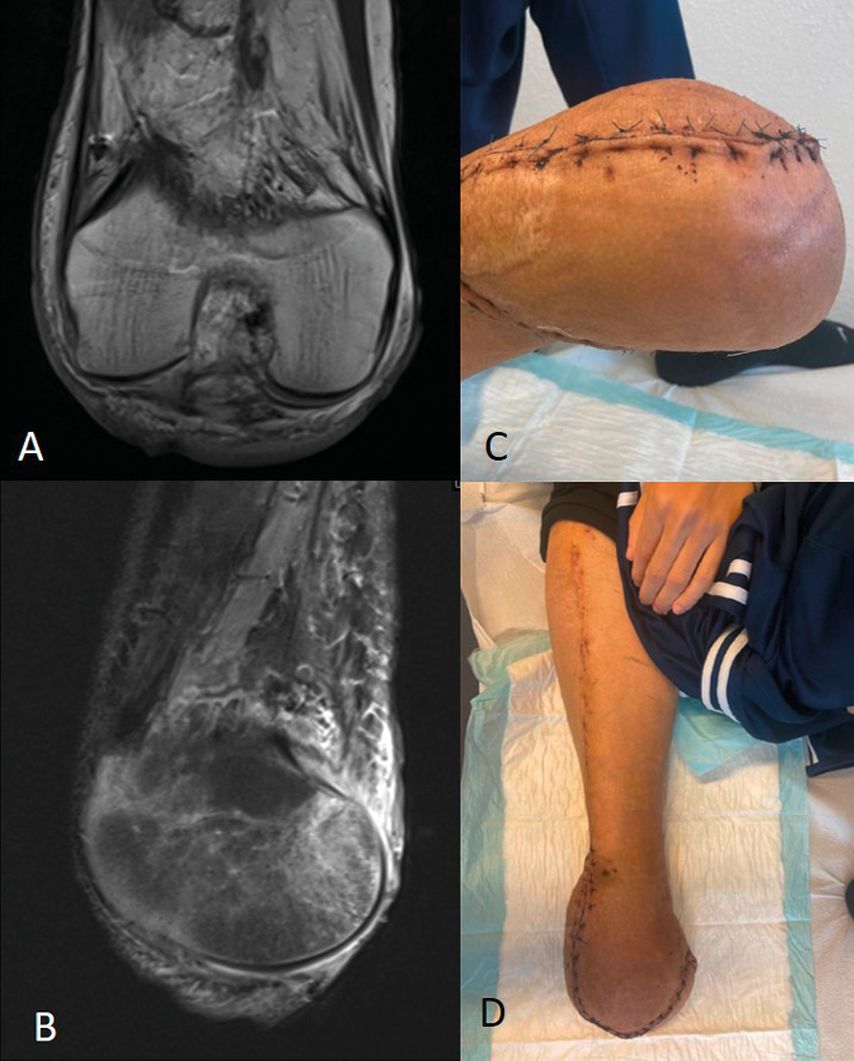
The first patient was a 22-year-old male with a second recurrence of a high-grade osteosarcoma of the right lower leg. The patient was treated initially in another hospital by tumor orthopedic surgeons. After multiple previous surgeries and preoperative chemotherapy, the knee had to be disarticulated because of the advanced tumor. Postoperatively a wound dehiscence at the lateral femoral condyle with exposed femoral condyle presented, when the patient was referred to our hospital. Since prosthetic fitting was planned, it was decided to perform a retrograde myocutaneous ALT flap for wound coverage and soft tissue augmentation. For improved soft tissue coverage, the vastus lateralis muscle was also elevated. The surgery was performed in cooperation between orthopedic and plastic surgeons. Intraoperative tissue sampling did not reveal signs for osteomyelitis. Three months after the surgery, the volume of the stump was stable, and therefore prosthetic fitting was started by technical orthopedic service (Fig. 1).
Fig. 1: A/B: This MRI image of a 22-year-old male shows poor soft tissue coverage on the residual limb after disarticulation of the knee, preventing him from fitting his prosthesis. C/D: The photographs show the clinical findings two weeks postoperatively after a retrograde myocutaneous ALT flap was performed to cover the soft tissue
Case II:
A 23-year old patient suffered a massive monotrauma of the left lower extremity being hit by a train. He sustained an open femur fracture Gustilo-Anderson grade III with injury of the femoral artery and an amputation of his foot on the ipsilateral side. After stabilization of the patient and initial fixation of the fracture with a external fixator, a femur nail was perfomed. To restore the soft tissue and function of the leg, a functional latissimus dorsi transfer was performed on the medial thigh to restore the adduction of the thigh. The course was complicated with wound infection. One year after the initial trauma, he still suffered from a septic pseudarthrosis. Although exchange of the metalwork was performed, a suppression therapy was needed because of an ongoing infection with candidas. For the whole decision-making process, the patient was presented several times at the IMSIK. In this meeting, it was decided to remove the metal work and treat the femoral pseudarthrosis with a free microvascular fibula to get rid of the suppression therapy. To obtain the best possible press-fit for initial optimal support, the osteotomies on the fibula as well as the resection on the femur were planed with 3D guides. After the initial planning, cutting guides were produced to plan the resection on the femur as well as for the fibula. After less than four months, the external fixateur could be removed with radiografically heald femur shaft and united graft. Unfortunately, after another 6 weeks, the patient sustained again a femur fracture on the distal end of the fibula after a weight lifting accident. A lateral plate was used to fix the fracture again. Intraoperative sampling didn’t show any sign of infection. After all, 6 months after the last surgery, the patient was able to walk again with lower leg prosthesis and the fracture had healed radiographically (Fig. 2).
Fig. 2: A/B:Radiological and clinical findings of an open Gustilo-Anderson grade III femur fracture after a rollover trauma caused by a train. The left foot was amputated, and replantation was not performed due to the multisegmental injury pattern. C/D: Radiograph 1 year after the initial trauma shows a septic pseudarthrosis of the femur. E: Metal removal and reconstruction with a free fibula were planned, and to achieve the best possible press fit for optimal initial support, the osteotomies on the fibula and resection on the femur were planned with 3D templates. F: Postoperative radiographs showing a free fibula reconstruction. An external fixator was used for further stabilization.
Case III:
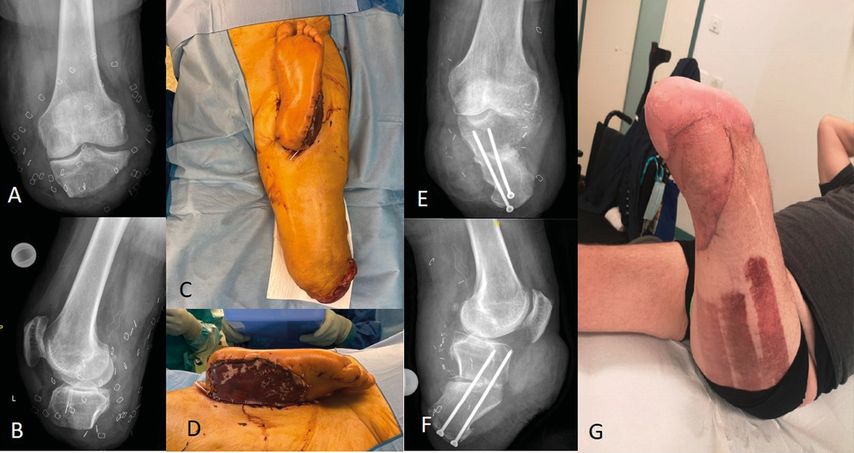
A 66-year old patient suffered a bilateral lower limb trauma with multi-fragment lower leg fracture on the right side and an amputation of the lower leg on the left side, distal to the knee joint. The foot below the ankle was protected and preserved in a shoe. The Plastic Surgery team was involved in addition to the trauma surgeons, directly in the emergency room. After the patient was stabilized systemically, fracture treatment of the right leg was prioritized with stabilization, the left leg amputation was completed and a heterotopic replantation of the intact left foot was performed - end to side on the lateral circumflex femoris artery. Five days after the intial trauma, definitive fixation was performed to treat the right tibia fracture. After further three days, the residual left stump was lengthened with an osteocutaneous fillet flap including a vascularized calcaneus and the extensor tendon apparatus of the knee was reconstructed with the plantar fascia of the replanted foot. Additionally, the lateral collateral ligament was reconstructed and an epineural coadaptation beween the tibial and sural nerve was performed. Clinically the patient showed early mobility of the knee after two months. At nine month follow-up the patient could full-weight bearing the leg with fluid gait and complete bone healing on the reconstructed left stump (Fig. 3).
Fig. 3: A/B: Radiographs of a 66-year-old patient after a traumatic below the knee amputation with a short tibial segment. C/D: Initial surgery with an orthoplastic team included heterotopic replantation of the intact left foot. E/F: Radiographs showing lengthening with an osteocutaneous fillet flap with vascularized calcaneus. G: At clinical follow-up after two months, the patient was able to flex and extend the knee
Conclusion
The concept of the orthoplastic approach brings together the strengths of orthopaedic surgery and other principles of plastic surgery to maximize outcomes in patients with severe extremity conditions. Ideally, this collaboration should be initiated as early as possible, e.g. in the trauma room and continued during follow-up, to achieve the best functional outcome for the patient.
Literatur:
1 Levin LS: The reconstructive ladder: an orthoplastic approach. Orthopedic Clinics of North America 1993; 24(3): 393-409 2 Mendenhall SD et al.: A review on the orthoplastic approach to lower limb reconstruction. Indian Journal of Plast Surg 2019; 52(1): 17-25 3 Carrel D: Operative technic of vascular anastomoses and visceral transplantation. Lyon med 1964; 212; 1561-8 4 Jacobson JH: Microsurgery in anastomosis of small vessels. Surg Forum. Vol. 11. 1960 5 Tamai S: History of microsurgery. Plastic and Reconstr Surg 2009; 124.6S e282-e294 6 Klifto MK et al.: The value of an orthoplastic approach to management of lower extremity trauma: systematic review and meta-analysis. Plast Reconstr Surg Glob Open 2021; 9(3): e3494 7 Hoyt BW et al.: Institutional experience and orthoplastic collaboration associated with improved flap-based limb salvage outcomes. Clin Orthop Relat Res 2021; 479(11): 2388-96 8 Boriani F et al.: Orthoplastic surgical collaboration is required to optimise the treatment of severe limb injuries: a multi-centre, prospective cohort study. J Plast Reconstr Aesthet Surg 2017; 70(6): 715-22 9 Nanchahal J: Standards for the management of open fractures of the lower limb. Royal Society of Medicine Press Limited 2009; 10 Fischer MD et al: The timing of flap coverage, bone-grafting, and intramedullary nailing in patients who have a fracture of the tibial shaft with extensive soft-tissue injury. JBJS 1991; 73(9): 1316-22 11 Gopal S et al.: Fix and flap: the radical orthopaedic and plastic treatment of severe open fractures of the tibia. JBJS 2000; 82(7): 959-66 12 Jenkinson RJ et al.: Delayed wound closure increases deep-infection rate associated with lower-grade open fractures: a propensity-matched cohort study. JBJS 2014; 96(5): 380-6 13 Fernandez MA et al.: The impact of a dedicated orthoplastic operating list on time to soft tissue coverage of open lower limb fractures. Ann R Colll Surg Engl 2015; 97(6): 456-9 14 Bosse MJ et al.: A prospective evaluation of the clinical utility of the lower-extremity injury-severity scores. JBJS 2001; 83(1): 3-14 15 Ly TV et al.: Ability of lower-extremity injury severity scores to predict functional outcome after limb salvage. J Bone Joint Surg Am 2008; 90(8): 1738-43 16 MacKenzie EJ, Bosse MJ: Factors influencing outcome following limb-threatening lower limb trauma: lessons learned from the Lower Extremity Assessment Project (LEAP). J Am Acad Orthop Surg 2006; 14(10): S205-S210 17 Lerman O Z et al.: The respective roles of plastic and orthopedic surgery in limb salvage. Plast Reconstr Surg 2011; 127 01:215S–227S 18 Zeller J et al.: Efficacy and safety of microsurgery in interdisciplinary treatment of sarcoma affecting the bone. Front Oncol 2019; 9:1300 19 Viñals JM et al.: Indications of microsurgery in soft tissue sarcomas. J Reconstr Microsurg 2012; 28(9): 619-25 20 Koulaxouzidis G et al.: Soft tissue sarcomas of the arm—oncosurgical and reconstructive principles within a multimodal, interdisciplinary setting. Front Surg 2016; 3: 12 21 Götzl R et al.: The role of plastic reconstructive surgery in surgical therapy of soft tissue sarcomas. Cancers (Basel) 2020; 12(12): 3534
Das könnte Sie auch interessieren:
Gezielte Diagnostik, bessere Therapie: gründliche Anamnese als Grundlage
Was rät man Eltern von Neugeborenen, wie sie eine atopische Dermatitis (AD) bei ihrem Baby verhindern können? Wann macht eine komponentenbasierte Allergiediagnostik Sinn? Wie lassen sich ...
Biologika-Therapie: Pipeline und Klinik
Biologika bieten die Option, in die hinter der atopischen Dermatitis stehenden Immunprozesse gezielt einzugreifen. Dieser Weg wurde zuerst mit dem Anti-IL-4/IL-13-Antikörper Dupilumab ...
Die menschliche Haut in der modernen Kunst
Dr. Ralph Ubl, Professor für neuere Kunstgeschichte an der Universität Basel, stellte sich der schwierigen Herausforderung, einem Raum voller erwartungsvoller Dermatologen das Organ Haut ...