PAD – dual antiplatelet or dual pathway antithrombotic therapy after endovascular therapy?
Autors:
Univ.-Prof. Dr. Marianne Brodmann
Dr. Katharina Gütl
Dr. Viktoria Muster
Division of Angiology
Medical University Graz, Austria
E-Mail: marianne.brodmann@medunigraz.at
Sie sind bereits registriert?
Loggen Sie sich mit Ihrem Universimed-Benutzerkonto ein:
Sie sind noch nicht registriert?
Registrieren Sie sich jetzt kostenlos auf universimed.com und erhalten Sie Zugang zu allen Artikeln, bewerten Sie Inhalte und speichern Sie interessante Beiträge in Ihrem persönlichen Bereich
zum späteren Lesen. Ihre Registrierung ist für alle Unversimed-Portale gültig. (inkl. allgemeineplus.at & med-Diplom.at)
In 2021 endovascular treatment (EVT) is routinely used to treat peripheral PAD. There is little direction to guide the best postinterventional care mainly based on experts consensus statement.1 Dual antiplatelet therapy (DAPT) – mainly aspirine and clopidogrel – is currently widely used after peripheral EVT in the hope of prolonging the patency of the intervention, especially in the crucial time period of endothelial healing.2
Keypoints
-
There is no convincing and overwhelming objective data to support daily practice DAPT (mainly Clopidogrel + ASA) after EVT and especially not after modern-world EVT.
-
Data we have are outdated.
-
The most robust data for DAPT are mainly from conservative trials.
-
The only solid data set representing the EVT space in PAD is the VOVAGER data.
Despite the popularity of DAPT, there is a lack of randomised controlled trials (RCT) in PAD literature to guide the optimum dose or the optimum length. Data are extrapolated from the results of RCTs in coronary interventions (PCIs). However, the DAPT regimen used in the treatment of coronary artery disease (CAD) cannot necessarily be extrapolated to the treatment of PAD, because platelet reactivity, plaque morphology, length of lesions treated, and vessel flow characteristics are substantially different in coronary arteries compared with lower extremity vessels. Besides that devices used in PAD intervention differ from coronary interventions (different drugs).
Another important gap is with regard of the evidence of duration of DAPT:
-
The choice, dose, and duration of antithrombotic drug therapy in relation to endovascular procedures is unclear.
-
DAPT is often used after endovascular procedures with large variability regarding its duration, usually between 1 and 3 months.3
-
The ESC guidelines on PAD recommend DAPT (aspirin + clopidogrel) for at least 1 month after infra-inguinal stent implantation.4
So how looks reality?
In different trial protocols where new devices are evaluated it says: Use DAPT with regard to the “standard of care” at the institution.
As already mentioned data for antiplatelet therapy cannot be extrapolated from coronary to the peripheral arteries, as there is a different mode of action. Higher residual platelet reactivity in response to adenosine diphosphate and arachidonic acid were found in LEAD vs. CAD patients. Patients undergoing peripheral angioplasty may have a weaker response to aspirin and clopidogrel compared to percutaneous coronary intervention patients.5 This has also be confirmed in the MIRROR trial where patients undergoing peripheral interventions were randomized in 2 arms (DAPT vs aspirine and placebo). Patients who showed a higher rate of reinterventions in the DAPT arm were all clopidogrel non-responders.6
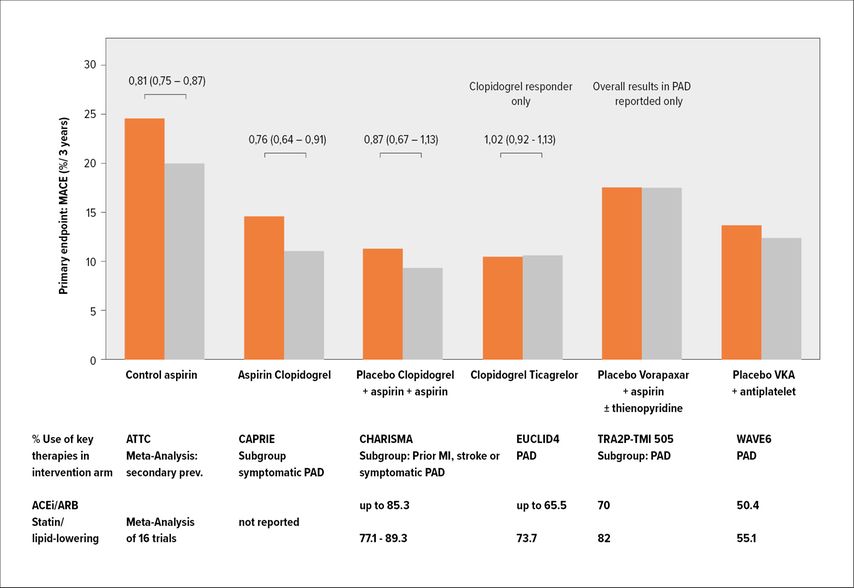
Another important aspect about the use of DAPT is the fact that it increases bleeding substantially. This has been shown in all the studies where different DAPT regimes have been evaluated in PAD patients (Fig. 1).
Fig. 1: Different trials which have evaluated DAPT in chronic PAD patients have shown an increased bleeding risk associated with DAPT, which has outweighed the beneficial effect
Schindewolf M and al. have looked recently into this topic specifically in patients with PAD and revascularization procedures and conducted a systematic „literature review of randomized trials comparing antithrombotic therapy following revascularization procedures in patients with peripheral artery disease“.7 Their conclusion was that generally, major bleeding rates were lower in SAPT (6.4%) versus DAPT trials (1.7%-8.4%).
Another important aspect with regard to DAPT data is that data supporting daily practice DAPT (Clopidogrel+ASA) are mainly not representing EVT procedures.1
How does EVT in PAD look today in 2021?
It is a great aera of innovation as there is an unmet need to improve EVT procedures in PAD with new devices and concepts. All these new technologies face “old-fashioned” adjunctive therapy. In contrary for CAD different antiplatelet strategies have been tested for different device technologies. This is for sure not the case in PAD.
Dual pathway inhibition by antithrombotic treatment with a direct oral anticoagulant (vascular dose of rivaroxaban 2,5mg twice daily and aspirine 100mg once daily) has shown a completely new approach for PAD patients. This has first been proven in the COMPASS trial, where especially patients with PAD (subgroup) have shown an overwhelming benefit with regard to different outcome endpoints: major cardiac events, major limb events and many more.8
The next step was evaluating this regime in patients who underwent revascularization for PAD. This was done in the VOYAGER trial. The outstanding issue about the VOYAGER trial is that these data really reflect modern therapeutic options for PAD patients:
-
no limitations for any kind of EVT technique which was available
-
drug coated balloons on the market
-
BMS (bare metal stent) on the market
-
DES (drug-eluting stent) on the market
-
atherectomy devices on the market
-
and, very important, 1/3 of the patients included were treated with open surgery.
In the VOYAGER trial it was clearly proven that with the dual pathway inhibition concept it was possible to reduce acute limb ischemia, major limb amputation, cardiovascular death, myocardial infarction and ischemic stroke significantly.
For us as vascular physicians it was eye-opening that this was the first antithrombotic regime that improved besides cardiovascular outcomes the limb outcomes in a significant way, regardless what kind of revascularization procedural approach was chosen.
Literatur:
1 Aboyans V. et al.: Eur Heart J 2021; 00: 1-16 2 Beiswenger AC et al.: J Vasc Surg 2018; 67: 1922-32 3 Olinic DM et al.: Antithrombotic treatment in peripheral artery disease. Vasa 2018; 47: 99-108 4 Aboyans V et al.: 2017 ESC Guidelines on the Diagnosis and Treatment of Peripheral Arterial Diseases, in collaboration with the European Society for Vascular Surgery (ESVS). Eur Heart J 2018; 39: 763-816 5 Gremmel T et al.: Response to antiplatelet therapy and platelet reactivity to thrombin receptor activating peptide-6 in cardiovascular interventions: differences between peripheral and coronary angioplasty. Atherosclerosis 2014; 232: 119-24 6 Tepe G et al.: Management of peripheral arterial interventions with mono or dual antiplatelet therapy – the MIRROR study: a randomised and double-blinded clinical trial. Eur Radiol 2012; 22: 1998-2006 7 Schindewolf M et al.: Angiology 2020: 71(9): 773-90 8 Anand SS et al.: J Am Coll Cardiol 2018; 71: 2306-15
Das könnte Sie auch interessieren:
ESC gibt umfassende Empfehlung für den Sport
Seit wenigen Tagen ist die erste Leitlinie der ESC zu den Themen Sportkardiologie und Training für Patienten mit kardiovaskulären Erkrankungen verfügbar. Sie empfiehlt Training für ...
ESC-Guideline zur Behandlung von Herzvitien bei Erwachsenen
Kinder, die mit kongenitalen Herzvitien geboren werden, erreichen mittlerweile zu mehr 90% das Erwachsenenalter. Mit dem Update ihrer Leitlinie zum Management kongenitaler Vitien bei ...
Inclisiran bei Patienten mit Statinintoleranz wirksam und sicher
Eine Analyse statinintoleranter Patienten aus dem Phase III Studienprogramm ORION zeigt, dass Inclisiran die LDL-Cholesterinspiegel kardiovaskulärer Hochrisikopatienten, die kein Statin ...