Advanced MRI techniques in hip cartilage assessment
Authors:
Dr. med. Malin Kristin Meier1,2
Dr. med. univ. José Andrés Roshardt2
Prof. Dr. med. Simon Damian Steppacher2
Dr.med. Florian Schmaranzer1,3
1Abteilung für diagnostische, interventionelle undpädiatrische Radiologie,
Inselspital Bern
2Abteilung für orthopädische Chirurgie,
Inselspital Bern
3Abteilung für Radiologie,
Universitätsspital Balgrist, Zürich
Korrespondierender Autor:
Dr.med. Florian Schmaranzer
E-Mail: florian.schmaranzer@insel.ch
Sie sind bereits registriert?
Loggen Sie sich mit Ihrem Universimed-Benutzerkonto ein:
Sie sind noch nicht registriert?
Registrieren Sie sich jetzt kostenlos auf universimed.com und erhalten Sie Zugang zu allen Artikeln, bewerten Sie Inhalte und speichern Sie interessante Beiträge in Ihrem persönlichen Bereich
zum späteren Lesen. Ihre Registrierung ist für alle Unversimed-Portale gültig. (inkl. allgemeineplus.at & med-Diplom.at)
Hip deformities are the main cause of hip pain and osteoarthritis in young adults, oftentimes necessitating hip-preserving surgery or, in more severe cases, a hip replacement. In order to successfully perform these surgeries and ensure the best possible outcome, surgeons rely on various imaging techniques. However, these techniques only produce 2D images which fail to accurately depict the complex 3D anatomy of the hip, and composing 3D models out of 2D images is a very time-consuming process. New technologies and techniques are applied in an attempt to automate 3D imaging and make it more convenient and reliable for hip cartilage assessment.
Challenges in joint preserving hipsurgery
Hip deformities, such as femoroacetabular impingement (FAI) and developmental dysplasia of the hip (DDH), are leading causes of hip pain and early osteoarthritis in young adults, often resulting in the need for total hip replacement.1 FAI is caused by an early bony conflict between the pelvis and femur which results from osseous deformities and damages the labrum and cartilage over time. In DDH, inadequate coverage of the femoral head by the acetabulum leads to increased stress to the acetabular rim. Hip-preserving surgeries aim to correct these deformities and improve joint biomechanics, potentially delaying joint degeneration. However, challenges remain.
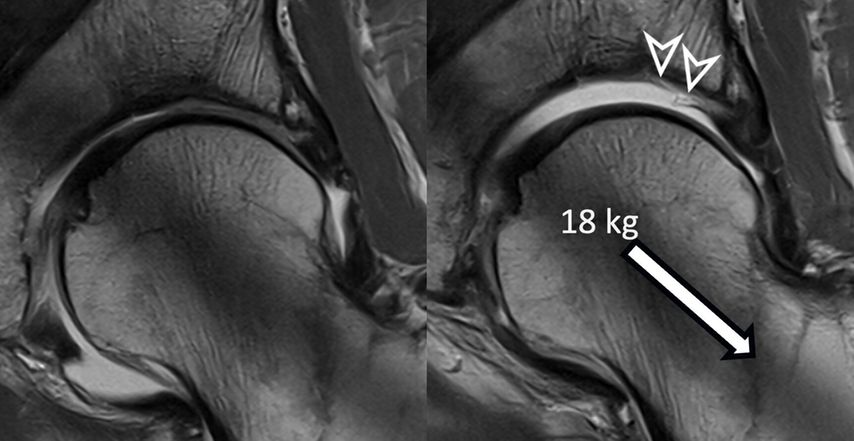
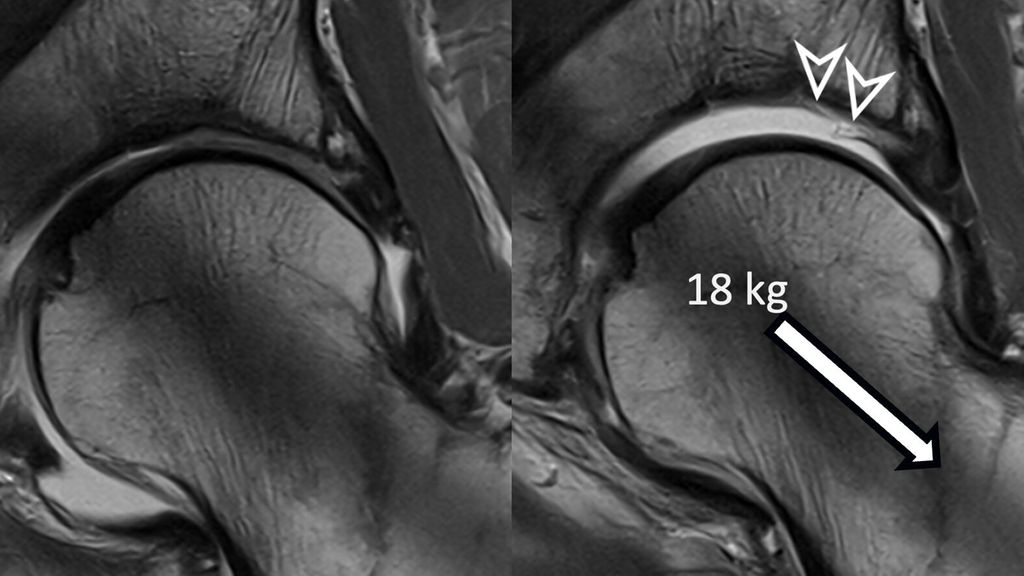
Fig. 1: Traction MR arthrography allows for better visualization of the opposing acetabular and
One challenge is to determine whether patients with early to moderate degeneration would benefit more from hip-preserving surgery or if hip replacement might be the favorable option based on already too severe joint deterioration.2 The other challenge is to accurately diagnose hip deformities. Depending on the underlying pathology, i.e. instability or hip impingement, different surgical techniques need to be considered. In cam-type FAI the aspherical portion at the femoral head-neck junction is resected. In pincer-type FAI there is a range of different degrees of acetabular overcoverage with or without a retroverted but presumably normally sized acetabular cup. Surgical treatment of pincer FAI may be either resection of the too deep acetabulum or correcting the retroverted acetabulum with anteverting periacetabular osteotomy which is a more complex and invasive surgery. Thus accurate diagnosis of the underlying deformity is crucial to achieve good outcome. The two major morphologic pathologies leading to hip instability are hip dysplasia due to insufficient acetabular coverage and increased femoral version. In these patients a periacetabular osteotomy or femoral osteotomy can be considered. Identifying the underlying pathology with standard preoperative imaging remains a challenge, especially in combined or borderline pathologies such as borderline hip dysplasia with associated cam deformities. Advanced diagnostic tools and image postprocessing yield great potential for improving preoperative diagnosis and surgical outcome.
Current standard imaging in joint preserving hip surgery
Current standard imaging modalities for diagnosing structural hip deformities include radiographs, computed tomography (CT), and magnetic resonance imaging (MRI). Radiographs are the primary diagnostic tool and are used to classify the bony morphology based on acetabular coverage and orientation as well as initial assessment of femoral head-neck junction.3 However, they only provide a 2D view of the hip’s complex 3D anatomy, which can be affected by variations in imaging techniques and patient positioning.3 To visualize osseous hip anatomy in more detail, CT can be used to create fast 3D bone models for a thorough analysis of acetabular and femoral morphology but has limited use for visualization of soft tissue. By contrast MRI offers excellent soft tissue contrast and is the modality of choice in assessing cartilage and labrum damage.3 However, joint degeneration can only be detected at an advanced level with macroscopic structural damage to the hip cartilage and labrum. This assessment is more or less qualitative and is prone to inter-observer variability. Furthermore, even though 3D MRI-sequences are commonly performed for image reformation, the actual assessment of labrum and cartilage damage is performed on few selected 2D images since manual segmentation of 3D labrum and cartilage models is too time-consuming for clinical routine.
Traction MRI of the hip for improved detection of macroscopic cartilage damage
The hip is a ball-and-socket joint with the labrum dividing it into peripheral and central compartments. In standard MR arthrography, a contrast agent expands the hip capsule and flows into the central joint cavity through the acetabular notch. However, most of the contrast does not spread centrally due to the opposing femoral and acetabular cartilage layers, which typically prevent its accumulation unless there is significant cartilage damage. Therefore, visualizing acetabular cartilage delamination which represents a typical and frequent finding in patients with cam-type FAI is challenging with direct MR arthrography.4
To improve visualization of the central joint cavity during MR arthrography, axial leg traction can be applied, similar to the joint distraction needed during hip arthroscopy (Fig. 1). Traction MR arthrography of the hip has shown high accuracy in detecting chondrolabral lesions, ligamentum teres injuries, and intra-articular loose bodies and has demonstrated its value in predicting failure of FAI surgery.5–8 It is particularly helpful for better visualizing the extent of cartilage damage in older patients with mild radiographic joint degeneration and thus aid in surgical decision making. Traction MR arthrography can also detect unstable labral tears in patients with hip dysplasia and may aid in planning treatment for femoral head necrosis in young patients with early collapse and preserved joint space.4
Biochemical MRI for compositional quantification of cartilage damage
Cartilage integrity is a crucial factor for the success of joint-preserving surgery. Morphologic MRI, the current gold standard, can only detect joint degeneration at advanced stages when severe structural changes in the hip cartilage and labrum are already present.9 However, biochemical deterioration of cartilage, marked by the loss of glycosaminoglycans (GAG), occurs before these changes become visible on MRI. To address this limitation, biochemically sensitive MRI techniques like delayed gadolinium-enhanced MRI of cartilage (dGEMRIC) have been developed.10,11
GAG, a key component of healthy cartilage, is negatively charged, and its loss reduces the cartilage’s overall negative charge. In dGEMRIC, a negatively charged gadolinium contrast agent penetrates the cartilage as GAG levels decrease, reducing the T1 relaxation time, which can be measured in MRI. Thus, dGEMRIC provides a quantifiable biomarker of cartilage health. Early studies at 1.5 Tesla showed dGEMRIC’s potential to predict the risk of early failure after joint-preserving surgery.12,13 However, with the adoption of 3 Tesla MRI in clinical practice, field inhomogeneity issues emerged with the traditional dGEMRIC technique. To address this, more robust inversion-recovery-based method was developed for 3D dGEMRIC imaging (MP2RAGE).14 Despite these advancements, standard dGEMRIC analysis requires manual placement of regions of interest on select 2D images, making it time-consuming and user-dependent, which limits its routine clinical use.
AI-based 3D analysis of cartilage and labrum morphology and cartilage damage
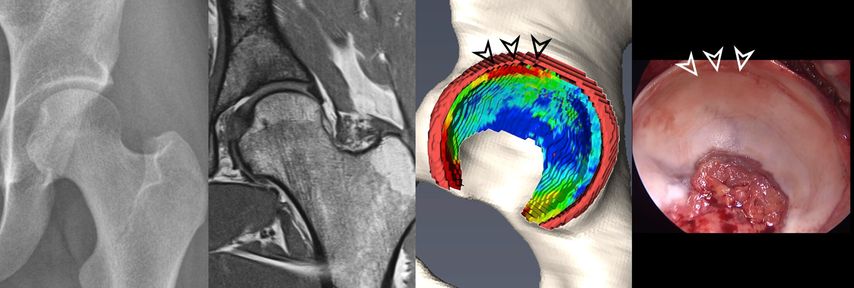
As mentioned above, hip MRI assessments are based on selected 2D images. Creating 3D models requires manual segmentation, which involves dividing an image into multiple regions of interest based on pixel properties. This process is done slice by slice, making it very time-consuming and impractical for routine clinical use and is affected by inter-observer variability even when performed by an expert. Deep learning, a branch of machine learning, has shown great promise in automating image segmentation. Convolutional neural networks, particularly those with U-net architecture, are commonly used for this purpose. More recently, the nnU-net, an extension of the U-net, was introduced. It automatically configures itself for biomedical image segmentation and has produced excellent results across various medical imaging tasks.15 Compared to other joints such as the knee automatic segmentation of hip cartilage is more challenging due to its naturally thinner structure and oblique orientation. Previous attempts to automate hip cartilage segmentation were based on small sample sizes and did not include the labrum.16–18 Ideally, combining a 3D analysis of chondro-labral morphology with cartilage composition would enable an improved analysis of chondro-labral dimensions and of the severity of joint damage (Fig. 2 & 3).
Fig. 2: 3D models of hip cartilage and labrum with color-coded dGEMRIC indices to visualize biochemical cartilage degeneration (red color, black arrowheads) which was confirmed during surgery (white arrowheads).
More recently, we introduced a deep-learning-based approach for automatic segmentation of hip cartilage and labrum using a 3D dGEMRIC sequence (MP2RAGE). The approach allows for automatic and reliable generation of 3D models of hip cartilage and labrum within seconds, and providing both 3D morphologic information of the hip joint as well as color-coded dGEMRIC indices for quantitative analysis of cartilage damage (Fig. 2 & 3).19
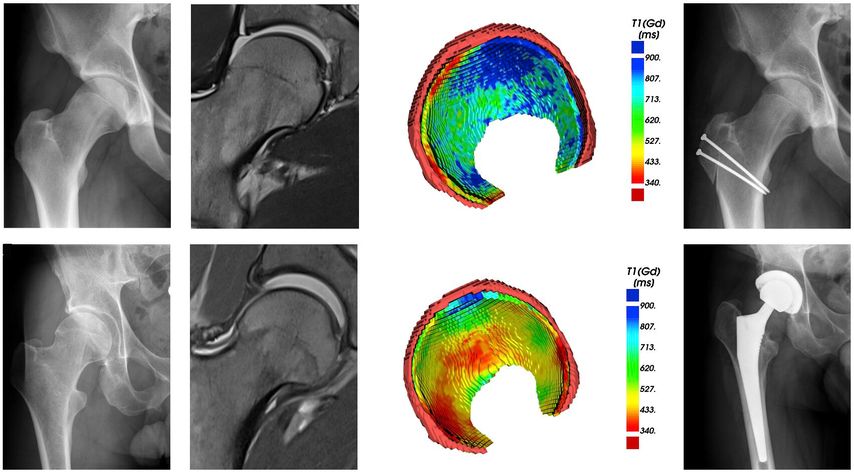
Fig. 3: Two patients with cam deformity of the proximal femur. Pelvic X-ray shows in both cases only mild arthritic changes. The morphologic MRI only allows 2D morphologic assessment of damage. The 3D cartilage models allow for a quantitative and 3D assessment of cartilage degeneration. Compared to the patient with good cartilage quality (blue color coding) who underwent impingement surgery the patient below showed too advanced signs of cartilage damage (red color coding) and thus underwent total hip replacement.
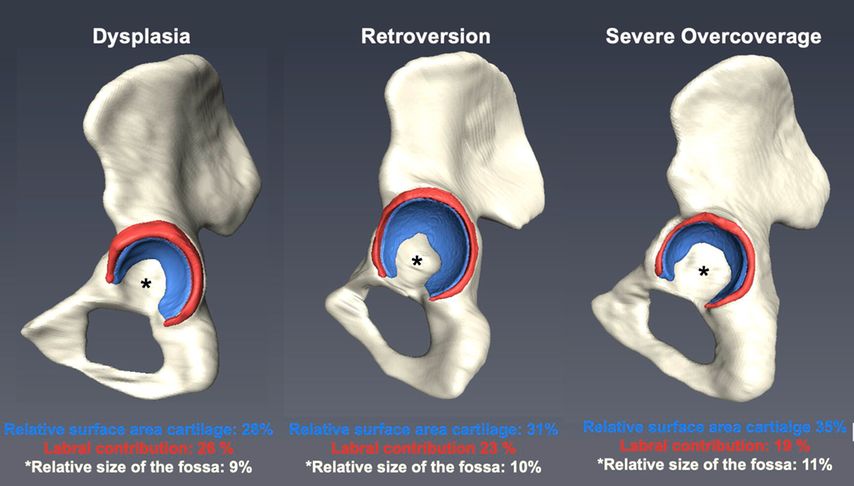
This new technique allows for the first time to investigate the 3D morphology of hip deformities based on MRI (Fig.4). Using this technology enabled us to quantify the size of the articular surface and demonstrate that the severely retroverted acetabulum does not actually represent a deep hip. Instead hips with acetabular retroversion present a smaller articulating cartilage surface area but a comparably large non-articulating fossa acetabularis (Fig. 4). This finding supports anteverting periacetabular osteotomy over acetabular rim trimming in order to prevent iatrogenic hip dysplasia. Furthermore, we could quantify the adaptive hypertrophy of the acetabular labrum in hip dysplasia compared to hips with a normal acetabulum and pincer-type hips. A fast and reliable individual analysis of cartilage and labrum surface area compared to surface area of the non-articulating fossa acetabularis yields unprecedented ways to characterize hip morphology with the goal to improve surgical planning on a routine basis. Furthermore, a fully automated volumetric analysis of cartilage composition using 3D dGEMRIC maps may aid surgeons when contemplating.
Fig. 4: Demonstrated are 3D models of pelvic bone with cartilage (blue) and labrum (red) of three different hip pathologies. Relative surface area of cartilage and the fossa is defined as the absolute surface area of cartilage divided by the absolute surface area of the femoral head. Labral contribution is defined as the absolute surface area of the labrum divided by the surface area of the joint contact surface (surface area labrum + cartilage)
Literatur:
1 Ganz R et al.: Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res 2003; 417: 112-20 2 Lerch TD et al.: One-third of hips after periacetabular osteotomy survive 30 years with good clinical results, no progression of arthritis, or conversion to THA. Clin Orthop Relat Res 2017; 475(4): 1154-68 3 Tannast M et al.: Femoroacetabular impingement: radiographic diagnosis—what the radiologist should know. AJR Am J Roentgenol 2007; 188(6): 1540-52 4 Schmaranzer F et al.: Conventional and arthrographic magnetic resonance techniques for hip evaluation: what the radiologist should know. Semin Musculoskelet Radiol 2019; 23(3): 227-51 5 Schmaranzer F et al.: Diagnostic performance of direct traction MR arthrography of the hip: detection of chondral and labral lesions with arthroscopic comparison. Eur Radiol 2015; 25(6): 1721-30 6 Schmaranzer F et al.: MR arthrography of the hip with and without leg traction: assessing the diagnostic performance in detection of ligamentum teres lesions with arthroscopic correlation. Eur J Radiol 2016; 85(2): 489-97 7 Schmaranzer F et al.: Usefulness of MR arthrography of the hip with and without leg traction in detection of intra-articular bodies. Acad Radiol 2019; 26(9): e252-59 8 Lerch TD et al.: Are degenerative findings detected on traction MR arthrography of the hip associated with failure of arthroscopic femoroacetabular impingement surgery? Eur Radiol 2023; 34(6): 3555-65 9 Sutter R et al.: Hip MRI: how useful is intraarticular contrast material for evaluating surgically proven lesions of the labrum and articular cartilage? AJR Am J Roentgenol 2014; 202(1): 160-9 10 Jessel RH et al.: Radiographic and patient factors associated with pre-radiographic osteoarthritis in hip dysplasia. J Bone Joint Surg Am 2009; 91(5): 1120-9 11 Kim YJ et al.: Assessment of early osteoarthritis in hip dysplasia with delayed gadolinium-enhanced magnetic resonance imaging of cartilage. J Bone Joint Surg Am 2003; 85(10): 1987-92 12 Cunningham T et al.: Delayed gadolinium-enhanced magnetic resonance imaging of cartilage to predict early failure of Bernese periacetabular osteotomy for hip dysplasia. J Bone Joint Surg Am 2006; 88(7): 1540-8 13 Kim SD et al.: Anterior delayed gadolinium-enhanced MRI of cartilage values predict joint failure after periacetabular osteotomy. Clin Orthop Relat Res 2012; 470(12): 3332-41 14 Schmaranzer F et al.: Magnetization-prepared 2 rapid gradient-echo MRI for B1 insensitive 3D T1 mapping of hip cartilage: an experimental and clinical validation. Radiology 2021; 299(1): 150-8 15 Isensee F et al.: nnU-Net: a self-configuring method for deep learning-based biomedical image segmentation. Nat Methods 2021; 18(2): 203-11 16 Li Z et al.: Entropy and distance maps-guided segmentation of articular cartilage: data from the Osteoarthritis Initiative. Int J Comput Assist Radiol Surg 2022; 17(3): 553-60 17 Ruckli AC et al.: Automated quantification of cartilage quality for hip treatment decision support. Int J Comput Assist Radiol Surg 2022; 2011-21 18 Schmaranzer F et al.: Automatic MRI-based three-dimensional models of hip cartilage provide improved morphologic and biochemical analysis. Clin Orthop Relat Res 2019; 477(5): 1036-52 19 Meier MK et al.: A deep learning approach for automatic 3D segmentation of hip cartilage and labrum from direct hip MR arthrography. Unpublished source 2023; https://doi.org/10.21203/rs.3.rs-3654066/v1
Das könnte Sie auch interessieren:
Neueste Entwicklungen der spinalen EndoskopieNachhaltige keramische Knochenimplantate bald aus dem 3D-Drucker
Die endoskopische Wirbelsäulenchirurgie hat sich von einer rein perkutanen Technik zu einer hochpräzisen, technisch ausgereiften Methode entwickelt, die ein weites Spektrum degenerativer ...
Seltene Kleingefässvaskulitiden im Fokus
Bei Vaskulitiden der kleinen Gefässe liegt eine nekrotisierende Entzündung der Gefässwand von kleinen intraparenchymatösen Arterien, Arteriolen, Kapillaren und Venolen vor. Was gilt es ...
Elektive Hüft-TEP bei Adipositas Grad III
Übergewichtige Patient:innen leiden früher als normalgewichtige Personen an einer Hüft- oder Kniearthrose. Allerdings sieht die aktuelle S3-Leitlinie zur Behandlung der Coxarthrose in ...