When is anatomic shoulder arthroplasty the best solution for patients over 65 years?
Authors:
PD Dr. med. Marc Schnetzke
Prof. Dr. med. Markus Loew
Deutsches Gelenkzentrum
Heidelberg, Germany
Correspondence:
E-Mail: marc.schnetzke@atos.de
Reverse shoulder arthroplasty (RSA) has become increasingly popular in patients over 65 years of age due to its independence from the integrity of the rotator cuff and good long-term results in recent years. There are theoretical advantages of RSA over total shoulder arthroplasty (TSA) in these patients. Nevertheless, even in patients over 65 years of age, it should be considered whether the patient could benefit from the use of a TSA compared to RSA.
Keypoints
-
In advanced OA with partial rotator cuff lesion and in B2 glenoids, good clinical outcome with TSA can be achieved even in elderly patients.
-
The clinical results of TSA tend to be better than those of RSA.
-
The complication and revision rates are lower with TSA than with RSA.
-
The revision possibilities according to TSA (especially for bone-sparing and convertible systems) are better than according to RSA.
-
The load-bearing capacity/return-to-sports rate after TSA is better than after RSA.
In an increasingly aging population with high functional demands, the number of implanted shoulder prostheses will continue to increase in the future.11 In recent years, the design of shoulder prostheses has developed in a trend-setting manner: Short-stem prostheses and stemless prostheses with metaphyseal fixation have replaced standard shaft prostheses with diaphyseal fixation.19 The clinical and radiological results of short-stem prostheses and stemless prostheses have been very promising so far: With comparably good clinical results and comparable complication and revision rates in the average follow-up available to date, the use of the bone-saving metaphysically fixed prostheses can facilitate a possible later revision.21,5
Beside the trend towards bone-saving implants, however, there is also a trend towards primary RSA in patients over 65 years of age.17 While different shoulder pathologies have been treated in the past with TSA and RSA, respectively, nowadays RSA is increasingly recommended instead of TSA in patients over the age of 65 in primary omarthritis (OA) with or without partial lesion of the rotator cuff and in dysplastic glenoids (type B2 Walch).9,1
Previous studies on TSA results have shown that secondary rotator cuff dysfunction occurs in approximately 17% of patients of all ages on average approximately 9 years after TSA, and that rotator cuff failure has been found to be the most common cause of early TSA failure.28 Another argument for routine implantation of RSA in patients over 65 years of age is the suspicion that pre-existing shoulder stiffness in OA could contribute to rotator cuff dysfunction despite intact rotator cuff tendons, and therefore might be associated with worse results.27
Therefore, it is reasonable to assume that many surgeons will consider the indication for RSA in patients over 65 years of age with primary OA regardless of the integrity of the rotator cuff in order to avoid the potential problem of rotator cuff insufficiency and therefore revision. In addition, RSA has good long-term results and the results after revision of TSA are heterogeneous.7
Current literature
In a recent study, Raval et al. examined the medium-term results after TSA with partial tear of the rotator cuff.15 The authors were able to show that patients over 75 years of age after TSA and partial tear of the rotator cuff can achieve good results. All patients examined reported an improvement in pain and objectively there was a significant improvement in postoperative range of motion. Despite the detected partial rotator cuff tear, the survival rate after 5–8 years was over 90%, which is comparable to the previously published survival rates for TSA with intact rotator cuff.14,23 The authors therefore concluded that, given the higher complications of RSA and the higher cost of implants, TSA in patients over 75 years of age with primary OA is a good indication even in the presence of a partial rotator cuff lesion.
In another recently published study, Edwards and co-workers compared the results of TSA and RSA in patients over 70 years of age.13 Especially in patients older than 70 years of age, no or only minimal differences were found in all outcome measures in early to mid-term follow-up. The most important result of the study was that patients over 70 years of age who received RSA were almost 4 times more likely to have a revision than patients who received TSA (8% vs. 2%). The authors therefore concluded that TSA and RSA may be equivalent in patients older than 70 years of age and that routine implantation of RSA is not recommended depending on the age of the patient.
Two previous studies comparing the results of TSA and RSA in older patients also found comparable results for the two procedures. Triplet et al. compared 18 TSA for primary OA and 33 RSA for cuff tear arthropathy in patients older than 80 years with a minimum follow-up of 2 years.24 Patients had comparable outcome in terms of pain, function and range of motion at follow-up, but there was a small but statistically significant advantage of TSA patients in the ASES score, satisfaction, length of hospital stay and blood transfusion rates. Wright et al. compared the clinical outcome of 102 TSAs and 33 RSAs for primary osteoarthritis with intact rotator cuff in patients over 70 years of age.27 After a mean follow-up period of 7 years, they also reported a comparable result in terms of function, pain, complications and revisions.
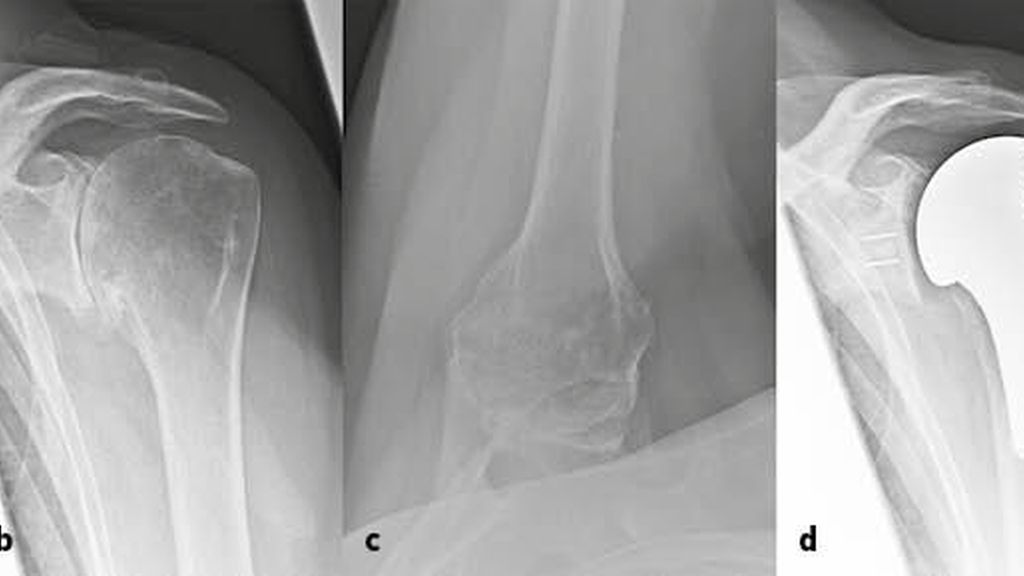
Overall, RSA is associated with a total complication rate of approximately 15%.3 In particular, infection rates are increased, with up to 4% described for RSA compared to 1.1% for TSA. In a recent register study with 17730 shoulder arthroplasties included, the infection rate for RSA in male patients was reported to be up to 8%.10 These data are also consistent with yet unpublished results of our own Shoulder Arthroplasty Register. The senior author of the current paper implanted a total of 217 TSA (mean age 68 years) and 158 RSA (74 years) between January 2013 and December 2019. Among the RSA patients were 16 patients (76 years) with primary OA in case of rotator cuff insufficiency or relevant glenoid deformity (glenoid type B2 according to Walch). Of these patients until now (12 to 84 months), 6 patients were revised after TSA (2,8%) and 17 patients after RSA (10,8%). Reasons for revision after TSA were one periprosthetic fracture and 3 infections. After RSA, 4 patients with wound hematoma and 1 patient with implant dislocation had early revision within 2 weeks after surgery. Late revisions were due to infections (7 cases) and implant complications, such as glenosphere loosening, component dissociation or periprosthetic fracture. Case study no.1 (Fig.1) shows the case of a 67-year-old female patient treated with TSA with primary OA, degenerative partial lesion of the supraspinatus tendon and a B2 glenoid according to Walch.
Fig. 1: Case study no. 1 shows the case of a 67-year-old female patient treated with TSA: a) Magnetic resonance imaging reveals a degenerative lesion of the supraspinatus tendon. b, c) Preoperative radiographs (anteroposterior and axial) show advanced primary OA with postoperative decentration of the humeral head in Walch’s type B2 glenoid. d, e) At 6-year follow-up, no radiological signs of bony adaptation around the stem and no signs of loosening of the glenoid are visible. At 6-year follow-up the patient is pain-free (0 of 15), the Constant Score is 78 points, the sex and age-adapted Constant Score is 122% and the Subjective Shoulder Value is 100%
Beside the integrity of the rotator cuff, the deformity of the glenoid has an influence on the choice of implant. Some authors recommend implanting RSA even with an intact rotator cuff in older patients with B2 glenoid deformity.4 The results of TSA in the presence of a relevant glenoid deformity are assumed to be associated with a higher rate of instability and glenoid loosening. However, recent studies show that reliable clinical and radiological results can also be obtained with TSA in the B2 glenoid. Magosch et al. recently published results from 48 patients (mean age 67 years) who were treated with TSA and a metal-back glenoid.8 Almost 30% of the patients had a B2 glenoid. After an average follow-up of 49 months, the clinical results of the patients with B1 and B2 glenoids were comparable. Glenoid loosening did not occur in any of the patients.
These results are consistent with our own experience. In our own patient population, a total of 17 patients (mean age 67 years) were treated with primary OA and a B2 glenoid using TSA and cemented all-polyethylene glenoid between 2013 and 2017. After 29 months of follow-up (24–38 months), the constant score improved from 30±6 to 75±6 points (p<0.001). Pain (5.1±3.6 to 14.4±0.9; p<0.001), subjective shoulder values (38±15% to 91±9%; p<0.001) and the range of motion for abduction, flexion and external rotation also improved significantly (p=0.002). No patient presented with radiologic glenoid loosening. Case study no.2 (Fig.2) shows the case of a 66-year-old male patient treated with TSA with primary OA and a B2 glenoid according to Walch.
Fig. 2: Case study no. 2 shows the case of a 66-year-old male patient treated with TSA: a) The axial plane of preoperative computed tomography shows the posterior decentration of the humeral head with glenoid type B2 according Walch. b, c) At 4-years follow-up no radiological signs of bony adaptation around the stem and no signs of loosening of the glenoid are visible. Good re-centring of the humeral head in the axial x-ray image. At 4-year follow-up the patient is pain-free (0 of 15), the Constant Score is 76 points, the sex and age-adapted Constant Score is 100% and the Subjective Shoulder Value is 92%
Based on our own experience and the literature data, we do not recommend to routinely perform RSA in primary osteoarthritis with intact rotator cuff solely due to age. While concerns regarding secondary rotator cuff insufficiency following TSA are justified, the studies show that successful results can be achieved with TSA even in the presence of a partial rotator cuff tear and that RSA may have a higher revision rate.
Return to sports
Another aspect that should be considered in the decision-making process is the resilience after implantation of a TSA or RSA. In the early weeks after surgery, RSA offers advantages over TSA. While TSA requires a 4–6 weeks immobilization due to the healing of subscapularis tendon, RSA can usually be treated with early functional rehabilitation. In the medium and long term, however, TSA is clearly superior to RSA in terms of resilience and functionality.
A good indicator for the functionality after a joint replacement is the sport ability after surgery. In a recently published meta-analysis, Papalia et al. have compared the sports ability after TSA and RSA.12 The authors reported that the return-to-sports rate after TSA and RSA in elderly patients was 82%, with 90% of patients after TSA and 77% of patients after RSA regaining their sports ability. Among the sports frequently performed after surgery, swimming has the highest return rate (84%), followed by fitness (77%), golf (77%) and tennis (69%).
How to achieve good outcomes with TSA
Compared to the RSA, the TSA represents a technically more advanced procedure. A vast experience of the treating surgeon with TSA is therefore necessary for good medium-term and long-term results. A number of technical aspects must be considered on both the humeral and glenoid side in order to achieve a good result with TSA.
When preparing the humeral component, the determination of the resection height, the resection angle and the retroversion requires more experience with TSA than with RSA.20 The principle here is to adhere to the given anatomy of the individual patient.18 Therefore, a freehand resection of the humeral head is legitimate, and special care must be taken to ensure that the attachments of the rotator cuff remain intact. Prior to resection of the humeral head, the osteophytes should be removed in order to perform a resection that is as correct as possible and is based on the natural anatomy of the patient. Another important aspect on the humeral side is the avoidance of overstuffing, which poses an increased risk of secondary rotator cuff insufficiency.6 The size of the humeral implant should be based on the size of the resected humeral head; in case of doubt, a smaller size should be selected to avoid overstuffing. Case no.3 (Fig.3) shows a 80-year-old female patient who has been treated with a stemless hemiarthroplasty for primary OA.
Fig. 3: Case no. 3 shows a 80-year-old female patient who has been treated with a stemless hemiarthroplasty: a) Preoperative anteroposterior radiograph shows a primary OA. b, c) At 6-month follow-up no radiological signs of bony adaptation around the humeral component
However, the weak link of TSA is not the stem but the glenoid component. On the glenoid side, the preparation of the glenoid and the cementing technique play an important role in the longevity of the glenoid component. In a prospective observational study, Raiss et al. showed that glenoid loosening occurs, in particular, in the long term.23 A patient cohort had a radiolucent line score 7 years postoperatively of 1.8, but there was a significant increase to 8.2 points after 13 years. These data show that glenoid loosening constitutes a relevant clinical problem.
The anatomy of the glenoid is highly variable, and insufficient allowance is made for this in traditional glenoid components with only one radius of curvature of the backside.25 Because of the variable anatomy of the glenoid, (almost) complete removal of subchondral bone is required in many cases in order to adapt the anatomy of the glenoid to the existing design of the glenoid component. However, preparation of the glenoid with the removal of subchondral bone has been identified as a substantial risk factor for the development of glenoid loosening.26 This was the rational for the development of new glenoid implants with variable backside curvature adapted to the individual anatomy. Previously, our study group has reported on 87 patients with primary OA and TSA with a short-stem prosthesis and cemented all-polyethylene glenoid.22 42 patients with a mean age of 67±8 years were treated with an all-polyethylene glenoid without variable curvature (group 1) and 45 patients with a mean age of 68±10 years were treated with an all-polyethylene glenoid with individualized curvature (group 2). After a mean follow-up of 31 months (range 24–50) the radiolucent line scores were 1.2±2.0 in group 1 and 0.9±1.1 in group 2 (p=0.410). In 5 patients (12%) from group 1 and 4 patients from group 2 (9%), the radiolucent line score increased over time. One patient in group 1 (2%) exhibited radiographic glenoid loosening. The all-polyethylene glenoid with individualized curvature showed promising short-term clinical and radiographic results. Further studies with a longer follow-up are necessary to evaluate whether the new all-polyethylene glenoid is superior to the standard all-polyethylene glenoid.
Finally, a solid technique of subscapular refixation is necessary for a good TSA result. Different procedures (tenotomy and osteotomy) with good results are described in literature.2,16 To sum up the results, it is important to have one solid technique and to immobilize the patients postoperatively accordingly to ensure a safe healing of the subscapularis.
Summary
In summary, while there certainly are expected and proven benefits of RSA in the elderly population, there are concerns about its routine use in indications that can also be treated with TSA. In addition to the increased complications, the implementation of routine use of RSA in this population may limit the revision options available to surgeons in the future. This is particularly true in light of the increasing popularity of anatomical shoulder prostheses with metaphyseal fixation, which better preserve bone stock and allow easier revision when needed.
References:
1 Alentorn-Geli E et al.: Reverse shoulder arthroplasty for patients with glenohumeral osteoarthritis secondary to glenoid dysplasia. Acta Orthop Belg 2019; 85(3): 274-82 2 Ameziane Y et al.: Single-row vs. double-row refixation of the subscapularis tendon after primary anatomic shoulder arthroplasty. Arch Orthop Trauma Surg 2020; online ahead of print 3 Barco R et al.: Complications in reverse shoulder arthroplasty. EFORT Open Rev 2016; 1(3): 72-80 4 Denard PJ, Walch G: Current concepts in the surgical management of primary glenohumeral arthritis with a biconcave glenoid. J Shoulder Elbow Surg 2013; 22(11): 1589-98 5 Erickson BJ et al.: Current state of short-stem implants in total shoulder arthroplasty: a systematic review of the literature. JSES Int 2020; 4(1): 114-9 6 Grubhofer F et al.: Does computerized CT-based 3D planning of the humeral head cut help to restore the anatomy of the proximal humerus after stemless total shoulder arthroplasty? J Shoulder Elbow Surg 2020; S1058-2746(20)30733-3; online ahead of print 7 Lehtimäki K et al.: Risk and risk factors for revision after primary reverse shoulder arthroplasty for cuff tear arthropathy and osteoarthritis: a Nordic Arthroplasty Register Association study. J Shoulder Elbow Surg 2018; 27(9): 1596-601 8 Magosch P et al.: Prospective midterm results of a new convertible glenoid component in anatomic shoulder arthroplasty: a cohort study. Arch Orthop Trauma Surg 2020; online ahead of print 9 Mizuno N et al.: Reverse total shoulder arthroplasty for primary glenohumeral osteoarthritis in patients with a biconcave glenoid. J Bone Joint Surg Am 2013; 95(14): 1297-304 10 Moeini S et al.: Reverse shoulder arthroplasty has a higher risk of revision due to infection than anatomical shoulder arthroplasty: 17730 primary shoulder arthroplasties from the Nordic Arthroplasty Register Association. Bone Joint J 2019; 101-B(6): 702-7 11 Padegimas EM et al.: Future patient demand for shoulder arthroplasty by younger patients: national projections. Clin Orthop Relat Res 2015; 473 (6): 1860-7 12 Papalia R et al.: Return to sport after anatomic and reverse total shoulder arthroplasty in elderly patients: a systematic review and meta-analysis. J Clin Med 2020; 9(5): 1576 13 Poondla RK et al.: Anatomic and reverse shoulder arthroplasty in patients 70 years of age and older: a comparison cohort at early to mid-term follow up. J Shoulder Elbow Surg 2020; S1058-2746(20)30711-4; online ahead of print 14 Raiss P et al.: Results of cemented total shoulder replacement with a minimum follow-up of ten years. J Bone Joint Surg Am 2012; 94(23): e171-10 15 Raval P et al.: Preoperative partial thickness rotator cuff tears do not compromise anatomical total shoulder replacement outcomes: medium-term follow-up. J Shoulder Elbow Surg 2020; S1058-2746(20)30632-7; online ahead of print 16 Scalise JJ et al.: Clinical, radiographic, and ultrasonographic comparison of subscapularis tenotomy and lesser tuberosity osteotomy for total shoulder arthroplasty. J Bone Joint Surg Am 2010; 92(7): 1627-34 17 Schairer WW et al.: National utilization of reverse total shoulder arthroplasty in the United States. J Shoulder Elbow Surg 2015; 24(1): 91-7 18 Schnetzke M et al.: Clinical and radiological results of a cementless short stem shoulder prosthesis at minimum follow-up of two years. Int Orthop 2015; 39(7): 1351-7 19 Schnetzke M et al.: Short-stem anatomical shoulder replacement—a systematic review. Obere Extremität 2019; 14(2): 139-48 20 Schnetzke M et al.: Anatomical and reverse shoulder replacement with a convertible, uncemented short-stem shoulder prosthesis: first clinical and radiological results. Arch Orthop Trauma Surg 2017; 137(5): 679-84 21 Schnetzke M et al.: Mid-term results of anatomical total shoulder arthroplasty for primary osteoarthritis using a short-stemmed cementless humeral component. Bone Joint J 2018; 100-B(5): 603-9 22 Schnetzke M et al.: Cemented all-polyethylene glenoid with standard or individualized backside curvature. Obere Extremität 2020; online ahead of print 23 Sowa B et al.: The medium- and long-term outcome of total shoulder arthroplasty for primary glenohumeral osteoarthritis in middle-aged patients. Bone Joint J 2017; 99-B(7): 939-43 24 Triplet JJ et al.: Anatomic and reverse total shoulder arthroplasty in patients older than 80 years. Orthopedics 2015; 38(10): e904-10 25 Walch G et al.: Three-dimensional assessment of the dimensions of the osteoarthritic glenoid. Bone Joint J 2013; 95-B(10): 1377-82 26 Walch G et al.: Patterns of loosening of polyethylene keeled glenoid components after shoulder arthroplasty for primary osteoarthritis: results of a multicenter study with more than five years of follow-up. J Bone Joint Surg Am 2012; 94(2): 145-50 27 Wright MA et al.: Comparison of clinical outcomes after anatomic total shoulder arthroplasty and reverse shoulder arthroplasty in patients 70 years and older with glenohumeral osteoarthritis and an intact rotator cuff. J Am Acad Orthop Surg 2020; 28(5): e222-9 28 Young AA et al.: Secondary rotator cuff dysfunction following total shoulder arthroplasty for primary glenohumeral osteoarthritis: results of a multicenter study with more than five years of follow-up. J Bone Joint Surg Am 2012; 94(8): 685-93
Das könnte Sie auch interessieren:
Neueste Entwicklungen der spinalen EndoskopieNachhaltige keramische Knochenimplantate bald aus dem 3D-Drucker
Die endoskopische Wirbelsäulenchirurgie hat sich von einer rein perkutanen Technik zu einer hochpräzisen, technisch ausgereiften Methode entwickelt, die ein weites Spektrum degenerativer ...
Seltene Kleingefässvaskulitiden im Fokus
Bei Vaskulitiden der kleinen Gefässe liegt eine nekrotisierende Entzündung der Gefässwand von kleinen intraparenchymatösen Arterien, Arteriolen, Kapillaren und Venolen vor. Was gilt es ...
Elektive Hüft-TEP bei Adipositas Grad III
Übergewichtige Patient:innen leiden früher als normalgewichtige Personen an einer Hüft- oder Kniearthrose. Allerdings sieht die aktuelle S3-Leitlinie zur Behandlung der Coxarthrose in ...





