Epidemiology and Economics: the two important e’s in diabEtEs
Author:
David Beran, MSc, PhD
Assistant Professor
Division of Tropical and Humanitarian Medicine
Faculty of Medicine
University of Geneva
E-mail: david.beran@unige.ch
Vielen Dank für Ihr Interesse!
Einige Inhalte sind aufgrund rechtlicher Bestimmungen nur für registrierte Nutzer bzw. medizinisches Fachpersonal zugänglich.
Sie sind bereits registriert?
Loggen Sie sich mit Ihrem Universimed-Benutzerkonto ein:
Sie sind noch nicht registriert?
Registrieren Sie sich jetzt kostenlos auf universimed.com und erhalten Sie Zugang zu allen Artikeln, bewerten Sie Inhalte und speichern Sie interessante Beiträge in Ihrem persönlichen Bereich
zum späteren Lesen. Ihre Registrierung ist für alle Unversimed-Portale gültig. (inkl. allgemeineplus.at & med-Diplom.at)
The epidemiology and the economic impact of diabetes are intimately intertwined. With the increase of the prevalence of type 2 diabetes this invariably not only impacts the health of the population, but also the costs to individuals and healthcare systems. From another perspective epidemiology and economics of diabetes are also linked in the fact that certain populations face higher rates of diabetes as well as worse outcomes due to barriers to access to care.
Keypoints
-
An understanding of epidemiology and economic factors related to diabetes is needed in order to develop effective policies and interventions and evaluate them.
-
The cost of diabetes for individuals and healthcare systems cannot be neglected.
-
Social determinants of health are important to be understood with more vulnerable populations facing an increased risk of diabetes, as well as poorer outcomes if they have diabetes.
-
In designing public health and healthcare system responses social determinants need to be considered to design appropriate measures for specific populations.
The burden of diabetes and its causes
The International Diabetes Federation (IDF) estimated that in 2021 there were 537 million people aged 20–79 with diabetes. This is estimated to increase by 46% globally between 2021 and 2045 with the majority of these additional cases in low- and middle-income countries (LMIC).1 In 2017 there were 9 million people with type 1 diabetes worldwide with an overall global increase in incidence of 3%.2 Parallel to this increase in the numbers of people with diabetes the costs of diabetes are increasing, with the IDF estimating that total health expenditure on diabetes was close to US$ 1000 billion in 2019.1 Beyond the costs of diabetes linked to the increasing numbers of people with the condition, complications, and new medicines and technologies, there is the need to consider how the economic situation of individuals might impact their risk of developing diabetes as well as their diabetes management if they have already diabetes.3 These so called social determinants of health include the environments where people are born, live and interact with different institutions including the healthcare system.
Social determinants of diabetes
In focusing on these determinants various factors such as ethnicity, being a migrant, racism, socio-economic position, education level and living in an urban or rural setting can all negatively impact the onset and the outcomes of diabetes. These different factors can affect incidence and prevalence trends, risk, access to health systems and medicines, as well as healthy lifestyles.
The lack of continuous access to enough food for a healthy life, defined as food insecurity, is more present in people with diabetes than in those without.4 This phenomenon impacts poorer individuals. Food insecurity is a risk factor for diabetes and has an impact on the management of diabetes. Being in a food-insecure environment can increase obesity and weight gain, as less healthy food is less expensive. For people with diabetes the high cost of healthcare and food might result in neglecting healthcare in favor of securing food supply. In addition, food insecurity can have an impact on mental health which also complicates diabetes management.
In the United States different social risk factors exist between black and white populations, resulting in prevalence of diabetes being 11% higher in black versus white Americans.5 The drivers of this difference are financial factors, food insecurity and unstable housing. In addition to epidemiological differences noted between different ethnic groups, epidemiology is important in disaggregating overarching ethnic groups into sub-groups to better understand factors linked with diabetes. For example overall prevalence of diabetes in the Asian population was 19,1% (NHANES data 2011–2016), however in looking at the different sub-populations within this overall category it was found that prevalence was significantly different in East Asians versus South Asians.6
Migration is another determinant to consider. This relates to factors of education, language, culture, and religion. These can all impact food and lifestyle practices as well as access to healthcare systems and the interactions with the system.7 Beyond these factors exposures prior to migration need to be considered, for example fetal or early-life malnutrition. Considerations also need to be given to how long the migrants have lived in their host countries and how their original culture has evolved to being closer to that of the country where they live, referred to as acculturation. This acculturation can relate to language proficiency as well as lifestyle with both positive and negative impacts. For example, fluency in the local language means no communication barriers regarding the healthcare system, but dietary changes possibly have a negative impact.
Racial disparities in diabetes prevalence are clearly the result of a variety of social determinants of health. Racism can also be seen as a social determinant of health with racial disparities both impacting the factors leading to diabetes, such as poverty and food security, but also, in regard of racism within healthcare institutions, impacting the responses certain populations receive from the healthcare system.8
Another disparity that is often ignored is that of urban versus rural populations. Traditionally, rural areas are perceived as being healthier than urban areas. However, a shift in mortality patterns occurred in the 1970s in the United States.9 This was caused by higher rates of smoking, hypertension and obesity, less leisure time physical activity as well as higher poverty rates. Beyond these factors there are also healthcare system-related barriers with less access to healthcare facilities.
The impact of these different factors on the onset and management of diabetes is presented in Figure1.
Access to diabetes care
Access to healthcare beyond geographic access or cultural/racial barriers is compounded by financial aspects. In some contexts, with Universal Health Coverage, costs are covered in part or fully by the government or insurance schemes meaning that the cost burden is not on the individual. However, in the United States regarding the uninsured population as well as in many LMIC the full cost of medicines and care is on the individual. In countries where there is no financial protection, poor and vulnerable populations will thus not be able to access and afford the care they need to manage their diabetes. In a study on admissions for diabetic ketoacidosis in an inner city setting in the United States it was found that in 68% the main cause was stopping insulin due to financial reasons.10 Lack of resources to afford insulin and other elements of diabetes care is also a problem in many LMICs: for example in Mali the full amount of the lowest paid government worker’s monthly salary is needed to pay for a month of diabetes care.11 In LMICs lack of access to insulin and diabetes care results in high rates of mortality. The fact that 100 years after the discovery of insulin many people still fail to access this life-saving medicine highlights the global inequity that exists between healthcare systems.
Conclusion
These epidemiological and economic factors are important to understand as for diabetes a life course approach is important, with social determinants shaping fetal, childhood and adolescent health and contributing to adult onset of diabetes. This is irrespective of the worrying increases in childhood obesity and type 2 diabetes. To address these disparities intensified efforts in social public health policies are required tackling economic, social, and environmental determinants of health. Responses are also needed for people with diabetes to ensure access to care, medicines and insulin. Healthcare system responses need to consider all the elements above and these measures need to address different sub-populations: people at risk of diabetes; obese individuals; people with impaired fasting glucose; those with undiagnosed diabetes; people with diabetes and those with complications. For innovations in this area it will be necessary to consider how wide social problems are addressed, just new pharmacological interventions are not enough.
Literature:
1 International Diabetes Federation: IDF Diabetes Atlas. 10th Edition. Brussels: International Diabetes Federation, 2021. 2 Green A et al.: Type 1 diabetes in 2017: global estimates of incident and prevalent cases in children and adults. Diabetologia 2021; 64: 2741-50 3 Seiglie JA et al.: To tackle diabetes, science and health systems must take into account social context. Nat Med 2021; 27: 193-5 4 Levi R et al.: Food insecurity and diabetes: overview of intersections and potential dual solutions. Diabetes Care 2023; 46: 1599-608 5 Vupputuri S et al.: The contribution of social-needs factors to racial differences in type 2 diabetes. Diabetes 2023; 72: 63-OR 6 Kanaya A: Diabetes in South Asians: Uncovering novel risk factors with longitudinal epidemiologic data. 2023. https://www.masalastudy.org/blog/2023/7/6/dr-kanaya-presenting-diabetes-in-south- asians-uncovering-novel-risk-factors-with-longitudinal- epidemiologic-data ; accessed November 24, 2023 7 European Association for Study of Diabetes: Immigration and diabetes. 2023. https://easd-elearning.org/about ; accessed November 29, 2023 8 Hill-Briggs F et al.: Social determinants of health, race, and diabetes population health improvement: Black/African Americans as a population exemplar. Curr Diab Rep 2022; 22: 117-28 9 American Diabetes Association: Researchers to review health data and rural populations. 2023. https://www.adameetingnews.org/live-updates/session-coverage/experts-to-review-health-data-and-rural-populations-in-u-s/ ; accessed November 27, 2023 10 Randall L et al.: Recurrent diabetic ketoacidosis in inner-city minority patients: behavioral, socioeconomic, and psychosocial factors. Diabetes Care 2011; 34: 1891-6 11 Abraimova A et al.: Management of type 1 diabetes in low- and middle-income countries: comparative health system assessments in Kyrgyzstan, Mali, Peru and Tanzania. Diabet Med 2022: e14891
Das könnte Sie auch interessieren:
Tachycardie supraventriculaire
Les tachycardies paroxystiques supraventriculaires régulières apparaissent généralement chez des patients sans cardiopathie structurelle. Dans cet article, nous discutons de l’importance ...
Risques du tabagisme pour la santé – sevrage tabagique
«Un fumeur avide qui lit et relit l’importance des risques du tabagisme pour sa santé cesse dans la plupart des cas ... de lire», avait déclaré Winston Churchill. «Le tabac est le seul ...
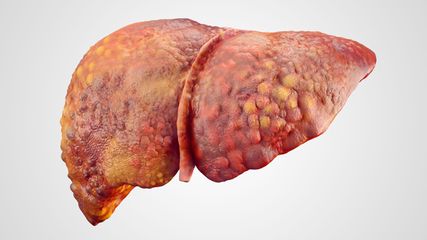
L’élastographie hépatique
En hépatologie, l’élastographie hépatique est l’instrument central de la prise en charge des patient·es atteint·es d’une maladie hépatique chronique. Les nouvelles conclusions permettent ...