Alpine Altitude Climate Treatment for Severe and Uncontrolled Asthma
Author:
Dr. Karin Fieten, PhD MSc MSc BSc
Research Fellow
Swiss Institute for Allergy and Asthma Research (SIAF)/Niederländisches Asthmazentrum Davos
Herman-Burchard-Strasse 9
7265 Davos Wolfgang
E-Mail: karin.fieten@siaf.uzh.ch
Sie sind bereits registriert?
Loggen Sie sich mit Ihrem Universimed-Benutzerkonto ein:
Sie sind noch nicht registriert?
Registrieren Sie sich jetzt kostenlos auf universimed.com und erhalten Sie Zugang zu allen Artikeln, bewerten Sie Inhalte und speichern Sie interessante Beiträge in Ihrem persönlichen Bereich
zum späteren Lesen. Ihre Registrierung ist für alle Unversimed-Portale gültig. (inkl. allgemeineplus.at & med-Diplom.at)
A significant proportion of patients with asthma remains uncontrolled, despite well-designed guidelines, effective pharmacological treatment and the increasing availability of biologicals. Suboptimal asthma control has a major impact on disease burden, quality of life and healthcare costs. Alpine altitude climate treatment (AACT) results in a rapid decrease in inflammation, and immunomodulatory downregulation, which enables the regain of asthma control as the basis for further improvement during multidisciplinary pulmonary rehabilitation.
Keypoints
-
AACT improves various outcomes such as asthma control and asthma-related quality of life, exacerbation rate and hospitalizations, oral corticosteroid reduction, lung function parameters, upper airways symptoms and exercise tolerance in adults and children based on observational studies, but there is a lack of randomized trials or studies with a control group supporting these observational findings.
-
The underlying mechanisms of AACT, including the influence of the physical characteristics of altitude, the environmental characteristics of the alpine climate, and the role of the multidisciplinary pulmonary rehabilitation program, are not yet fully understood.
-
AACT could be considered as treatment option for all patients with persistent uncontrolled asthma, despite maximum treatment according to guidelines.
Asthma is a chronic inflammatory airway disease, characterized by variable recurring symptoms, reversible airflow obstruction and airway hyperresponsiveness. Asthma symptoms include wheezing, chest tightness, breathlessness, and coughing. While asthma has an estimated global prevalence of ~334 million people, patients with severe asthma represent only 3% to 5% of this population.1 Asthma severity is assessed retrospectively from the level of required treatment to control symptoms and exacerbations. Managing severe asthma is a major challenge due to the heterogeneity of the disease, characterized by different clinical phenotypes and biological endotypes, and influenced by various comorbidities and risk factors.2 Severe asthma results in significant emotional, financial, functional and medication-related burdens.3
Many patients with severe asthma do not reach sufficient disease control and continue to experience daytime or nightly asthma symptoms, activity limitations and frequent exacerbations despite treatment with medium to high-dose inhaled corticosteroids (ICS) and long-acting β2 agonists (LABAs), plus a second controller with or without oral corticosteroids (OCS), according to GINA Step 4 or 5.4 Severe uncontrolled asthma accounts for a disproportionate use of asthma-related healthcare resource utilization and remains a significant unmet need in respiratory medicine.5
History of Alpine Altitude Climate Treatment
Historically, the treatment of pulmonary diseases at altitude, in the European alpine climate, developed from the treatment of tuberculosis. During the European tuberculosis epidemic in the 19th century, severely ill people were treated in mountain sanatoria. Their chances to survive the disease were naturally increased because of the treatment regimen that mostly consisted of several hours of rest and several meals a day. After the introduction of effective tuberculosis medication, the need for treatment in the mountain sanatoria reduced and most clinics closed, became hotels or changed their treatment concept to other pulmonary diseases like asthma or allergic diseases such as atopic dermatitis or chronic rhinosinusitis.
International treatment guidelines recommend a stepwise multidisciplinary approach for asthma management with the aim to achieve optimal disease control.1,4 Avoidance of environmental triggers, assessment of treatable traits, treatment of modifiable risk factors and comorbidities, non-pharmacological add-on therapies, identifying possible obstacles to medication adherence, checking inhaler technique, maintenance of daily physical activity, avoidance of triggers, education and skills training facilitate achieving asthma control and are important in the management of uncontrolled and severe asthma.1,4
Alpine altitude climate treatment (AACT) is designed for patients with uncontrolled severe or difficult-to-treat asthma and is mainly provided by specialized asthma clinics in central Europe (Switzerland, Italy, France, Germany). Currently available AACT programs for the treatment of uncontrolled asthma combine three elements: the physical characteristics of altitude, the environmental characteristics of the alpine climate and a personalized multidisciplinary pulmonary rehabilitation approach.6
Clinical and Inflammatory Outcomes
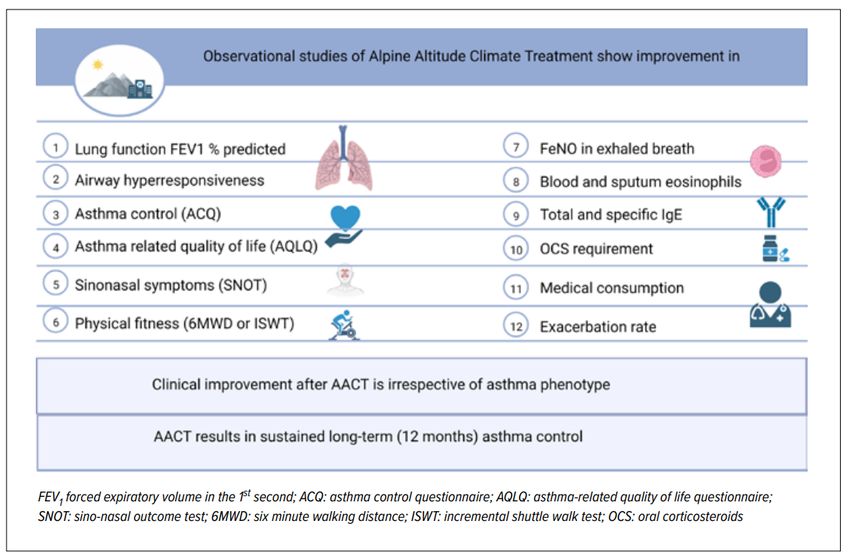
The recently published EAACI position paper on alpine altitude climate treatment identified 46 clinical studies using AACT as intervention and 2 systematic reviews with FEV1 and PC2O as outcomes.6 Most studies were observational without a control group. There was great study heterogeneity regarding treatment duration, patient population, altitude, and possibly regarding the contents of the pulmonary rehabilitation program. The observational studies demonstrated clinical and functional improvement of asthma parameters after AACT, such as improved asthma control, asthma related quality of life, improved lung function, less sinonasal symptoms, reduced need for OCS, less exacerbations and hospitalizations, improved physical fitness, and less fatigue (Fig. 1).6 These effects seem to last up to 12 months after the end of AACT.
One of the most striking observations during AACT are the rapid reduction of blood eosinophils and FeNO in exhaled breath, which is consistently reported across studies. Other studies showed a reduction of cytokines, such as IL-5, IL-10 and IL-13, suggesting that the type-2 inflammation, represented by ILC2 and Th2 cells and eosinophils, is reduced in patients with allergic asthma.7,8 Furthermore the suppressive and regulatory phenotype of regulatory T cells in all asthma phenotypes is restored.7
Fig. 1: Observational studies, as summarized in the EAACI Position Paper, demonstrate clinical and functional improvement of several asthma parameters after alpine altitude climate treatment. Further preferably randomized controlled studies are needed to corroborate these findings (created with Biorender.com)
Physical Altitude
With increasing altitude the barometric pressure drops, leading to reduced oxygen pressure, less air humidity, a generally lower air temperature and increased exposure to UV radiation. Less airway resistance facilitates breathing, increases inspiratory and expiratory air flow and reduces dynamic hyperinflation. This may lead to more effective physical training compared to sea level and may be an important mechanism of the improved physical fitness after AACT. A potentially important mechanism for the observed reduction in inflammation is the family of hypoxia-induced factors (HIF). They are expressed in various immune and tissue resident cells, such as eosinophils, neutrophils, innate lymphoid cells, and T cells, and have direct anti-inflammatory effects. The oxygen sensors in each cell are quite sensitive and it may be possible that upregulation of HIF already starts at the moderate altitudes where the European clinics are located, even though altitudes up to 2500m reduce the inspiratory oxygen pressure with 15 to 20% and there is little compensation needed for hypoxia. However, upregulation of HIF in patients within the first days of arrival at altitude has never been measured.
Environmental Exposure
Another important mechanism of effect may be the reduced environmental exposure (Fig.2). Various studies have shown that especially in uncontrolled asthma, environmental exposure to aeroallergens is important in disease exacerbations and symptoms. In the alpine climate, there is less exposure to aeroallergens, such as pollen, molds and house dust mites (HDM). There are generally less pollen, the pollen season is shorter and some pollen are completely absent at altitude. Ever since the identification of the house dust mite, it has been recognized as a major allergen source and environmental exposure to HDM has been linked to asthma-related symptoms. Less HDM with increasing altitude has been demonstrated since the 70s and allergen avoidance has long been thought to be the main mechanism of effect during AACT. However, more recent studies could not support the reduction in HDM with increasing altitude suggesting that other mechanisms apart from allergen avoidance are important for the observed decrease in inflammation.9
Fig. 2: Alpine altitude climate treatment for severe and uncontrolled asthma combines the physical characteristics of altitude, the environmental characteristics of the alpine climate and a personalized multidisciplinary pulmonary rehabilitation approach resulting in improved asthma control (created with Biorender.com)
The existing European altitude clinics are located in areas with low outdoor air pollution. Urbanization, industrialization and traffic-related air pollution, together with weather and landscape characteristics, determine the total amount of air pollution which is generally lower in alpine altitude villages.10 The exact mechanisms by which exposure to air pollutants influence asthma exacerbations are not completely clear.
Microbiome composition may also be influenced by the alpine environment or by the moderate altitude. During AACT a significant increase in microbial diversity on the skin of children with difficult-to-treat atopic dermatitis and asthma was observed, whereas such alpha diversity did not change in a control group treated at sea level.11 Several studies have demonstrated differences in the airway, nasal and gut microbiome between asthmatic patients and healthy subjects.12 Different microbial communities (environmental, gut, airways, nose) are able to interact with each other, regulate immune function and may also impact asthma development and severity.13
Furthermore stress is an important factor. There is a link between asthma severity and control, psychological aspects (such as subjective perception and coping style) and mental health. Psychologic comorbidities significantly influence asthma control and have substantial impact on quality of life in asthma. Anxiety and depression occur more frequently in patients with asthma and are associated with poorer asthma outcomes.14 Behavioral factors such as nonadherence and inadequate self-management skills have been associated with anxiety and depression.15
Furthermore, chronic stress has been shown to lead to biological changes, such as the expression of immunological genes, cytokine regulation, and cortisol levels, which may influence the pathophysiology of asthma and the therapeutic response in patients exposed to chronic stress.16 Therefore, regardless of the underlying cause, it is important to pay attention to chronic stress in patients with severe asthma and to look carefully at which therapy, practical support and coping strategies the patient needs to reduce stress. During AACT, patients avoid those psychosocial stress factors that are continually present in their usual environment by being away from home, work, and social environment. Furthermore, the patients receive psychological assessment and treatment of stress-related factors.
Pulmonary Rehabilitation
The stepwise multidisciplinary approach for asthma management includes referral to a specialized clinic to assess asthma phenotype and contributing factors.4 Pulmonary rehabilitation may be provided as an add-on treatment to provide self-management education, treat modifiable risk factors and comorbidities and other non-pharmacological therapies and strategies. A framework for systematic patient assessment is provided by the concept of treatable traits, divided into pulmonary, extra pulmonary and behavioral/lifestyle factors.17 Most pulmonary rehabilitation programs for severe asthma include an extensive multidimensional assessment resulting in a health profile that includes the asthma phenotype, pathophysiological features and all treatable traits. The main treatment goals of AACT are to achieve asthma control and to improve quality of life and daily functioning. Regaining asthma control allows for effective pulmonary rehabilitation with further physical and psychological improvement and makes it possible to taper off medication, such as high doses of ICS, OCS or SABA overuse.
Conclusion
From a clinical point of view, AACT could be considered as treatment option for patients with severe or uncontrolled asthma despite maximum treatment according to guidelines. These may be patients who do not respond to biologicals, who experience impaired quality of life, are dependent on oral steroids, have frequent exacerbations and hospitalizations, severely impaired lung function, marked upper airway symptoms, or decreased exercise tolerance. AACT is currently mostly provided to patients with severe uncontrolled asthma as a last resort, especially since the introduction of biologicals. The specific effectiveness of AACT may lie in the observed rapid decrease in inflammation and immunomodulatory downregulation which enables the regain of asthma control as the basis for further improvement during pulmonary multidisciplinary rehabilitation. The type 2 immune response, which is a significant driver of asthma pathology in eosinophilic and allergic asthma, is reduced during AACT. However, there is heterogeneity among patients in AACT treatment response and also in the sustainment of treatment effects, after patients return to their home environment. Further basic immunological and clinical research, with well-designed studies, will be necessary to further define which asthma phenotypes will benefit most from AACT and which patients will retain the effect most efficiently in their home environment.
Literature:
1 Chung KF et al.: International ERS/ATS guidelines on definition, evaluation and treatment of severe asthma. Eur Respir J 2014; 43 :343-73 2 Clark VL et al.: Multidimensional assessment of severe asthma: a systematic review and meta-analysis. Respirology 2017; 22: 1262-75 3Stubbs MA et al.: Living well with severe asthma. Breathe 2019; 15: e40-9 4 Global strategy for asthma management and prevention. 2022. www.ginasthma.org. (accessed 24.06.2022) 5 Israel E, Reddel HK: Severe and difficult-to-treat asthma in adults. N Engl J Med 2017; 377: 965-76 6 Fieten KB et al.: Alpine altitude climate treatment for severe and uncontrolled asthma: An EAACI position paper. Allergy 2022; 77: 1991-2024 7 Boonpiyathad T et al.: Impact of high-altitude therapy on type-2 immune responses in asthma patients. Allergy 2020; 75: 84-94 8 Quignon P et al.: Altitude healing effect in severe asthmatic children. Respir Med Res 2020; 79: 100810 9 Grafetstatter C et al.: No concentration decrease of house dust mite allergens with rising altitude in alpine regions. Allergy Asthma Immunol Res 2016; 8: 312-8 10 Guarnieri M, Balmes JR: Outdoor air pollution and asthma. Lancet 2014; 383: 1581-92 11 van Mierlo MMF et al.: The influence of treatment in alpine and moderate maritime climate on the composition of the skin microbiome in patients with difficult to treat atopic dermatitis. Clin Exp Allergy 2019; 49: 1437-45 12 Huang YJ, Boushey HA: The microbiome in asthma. J Allergy Clin Immunol 2015; 135: 25-30 13 Carr TF et al.: Microbiome in mechanisms of asthma. Clin Chest Med 2019; 40: 87-96 14 Thomas M et al.: Asthma and psychological dysfunction. Prim Care Respir J 2011; 20: 250-6 15 Cluley S, Cochrane GM: Psychological disorder in asthma is associated with poor control and poor adherence to inhaled steroids. Respir Med 2001; 95: 37-9 16 Barnthouse M, Jones BL: The Impact of environmental chronic and toxic stress on asthma. Clin Rev Allergy Immunol 2019; 57: 427-38 17 Agusti A et al.: Treatable traits: toward precision medicine of chronic airway diseases. Eur Respir J 2016 ;47: 410-9
Das könnte Sie auch interessieren:
Inklusivere Ansätze in der Behandlung von Lungenerkrankungen
Warum Intersektionalität und Barrierefreiheit Merkmale klinischer Qualität sind: Der vorliegende Beitrag fasst zentrale Inhalte des Vortrags „Inklusivere Ansätze in der Behandlung von ...
Seltene pulmonale Mykosen: Reisemitbringsel oder doch schon heimisch?
Endemische systemische Mykosen werden überwiegend durch Schimmelpilze verursacht, die im menschlichen Organismus charakteristische Hefeformen annehmen. Klima- und Landnutzungswandel ...