The use of ultrasonography to guide aesthetic filler injections
Authors:
Dr.med. Paula Bonavia
Dr.med. Roberta Vasconcelos-Berg, PhD
Margarethenklinik
Universitätsspital Basel
E-Mail: roberta.vasconcelos-berg@usb.ch
The use of aesthetic filler injections has been steadily increasing in recent years. Correspondingly, there has also been an increase in reported complications. Among these, vascular occlusion stands out as particularly concerning. While essential for the safe administration of injectable treatments, even comprehensive anatomical knowledge cannot fully eliminate the risks due to natural anatomical variation. High-frequency Doppler ultrasound allows practitioners to navigate facial structures safely during aesthetic injections and can be utilized to enhance the aesthetic and functional outcomes of treatments. Since 2020, the Margarethenklinik at the University Hospital of Basel has adopted ultrasound guidance for filler treatments.
Keypoints
-
Ultrasound guidance in aesthetic filler procedures may enhance safety by allowing real-time visualization of vascular structures, potentially reducing the risk of complications such as vascular occlusion and supporting more precise product placement.
-
While ultrasound-guided techniques require specialized training and anatomical knowledge, they offer the possibility of increased procedural safety, which may appeal to patients seeking secure aesthetic outcomes.
The availability of aesthetic filler injections on the internet, social media, and other media outlets is extensive, and a quick search reveals before-and-after images that promise rapid, straightforward results. However, these depictions often overlook the complexity and potential risks associated with the procedure.
Facial anatomy is intricate, and vascular anatomy—both venous and arterial—often coincides with common filler treatment areas. For instance, the facial artery lies directly beneath the nasolabial fold in approximately 70% of cases,1 while the angular vein is in the tear trough region, and the labial artery follows a «dolphin-like» trajectory, weaving in and out of the orbicularis oris muscle and varying in depth along the lips.2 Additionally, these vessels may vary in location from patient to patient. Notably, the internal and external carotid systems of the face connect at several points, meaning that a foreign substance like hyaluronic acid injected into any facial artery could potentially migrate through these anastomoses to the ocular vessels, resulting in occlusion and possible blindness.
The recent advancements in high-frequency ultrasound transducers have enhanced visualization of superficial layers, including the skin. Doppler ultrasound (DUS) enables real-time imaging of vascular structures, reducing the risk of intravascular injection or injection too close to a vessel, which can cause external compression. However, using DUS to guide procedures requires a learning curve for the injector, involving significant time and financial investment.
Investing in the development of this technique not only enhances the safety of the procedure but may also increase its precision, as the injector gains exact control over the product placement, potentially optimizing aesthetic outcomes. Furthermore, the perceived increase in procedural safety may attract new patients seeking these benefits.
Since 2020, the Margarethenklinik at the University Hospital of Basel has integrated ultrasound guidance into its filler treatments, treating approximately 400 patients.
This article aims to present an overview of our recommended approach to ultrasound-guided filler injections, offering practical guidance for clinicians who wish to start using this technique in their practice and outlining the practical aspects of utilizing Doppler Ultrasound (DUS) to guide the injection of fillers and biostimulators, as practiced in the Division of Aesthetic Dermatology at the University Hospital of Basel, Switzerland, since July 2020.
Selecting the appropriate ultrasound equipment
There are various types of ultrasound devices, and each should be selected based on the injector’s specific needs. The development of portable and more affordable devices has made it easier for practitioners to adopt this technology. Several key factors should be considered when choosing an ultrasound device and transducers for injections in the skin and subcutaneous tissues:
-
High-frequency linear transducers: To achieve optimal resolution with shallow penetration, a transducer with a frequency of at least 15MHz is recommended.3
-
Small footprint: This feature is particularly beneficial for scanning the face, which has irregular contours. Smaller transducers also allow better observation of skin color changes during injection, enabling rapid detection of any blanching.3
-
Color and power Doppler modes:These modes enable visualization of vascular flow, helping identify vascular structures accurately.3
Additional factors, such as the transducer’s weight, connection type (wired or wireless), cost, portability, and touch screen parameter control, may also influence equipment selection.
Regardless of the chosen device, it is essential to learn how to optimize parameters like depth penetration and gain to achieve the best possible image quality.
Material preparation
Importance of gel in sound conduction
In ultrasonography, gel serves as a coupling medium between the transducer and the skin. It eliminates the air that naturally exists between the transducer and the skin, as air is a poor conductor for ultrasound waves and would result in signal loss. In diagnostic dermatologic ultrasound, a generous amount of gel is used, which also helps prevent compression of the skin by the transducer—a factor that can interfere with anatomical measurements. For guided treatments, however, a thinner layer of sterile gel is typically applied; using too much gel would make the skin slippery and hinder the procedure.
Transducer cleaning and protection
To prevent contamination in the treatment area, it is essential to ensure both disinfection and sterile protection of the ultrasound transducers during guided procedures. Transducer cleaning is performed with specific non-alcoholic solutions designed for this purpose, often provided in pre-moistened wipes.
To maintain transducer sterility upon skin contact and to avoid contamination from blood or secretions, a sterile barrier is recommended during the procedure. The type of transducer protection depends on its size, with options including non-lubricated condoms, sterile finger gloves, or sterile plastic wraps (Fig. 1 a-c). For optimal sound wave conduction, gel must be applied both between the transducer and the protective covering, and between the covering and the patient’s skin.
Positioning of operators
In most cases, ultrasound-guided filler procedures are performed by the injector alone or with the help of a non-medical team member. In such situations, both hands must be used simultaneously, which requires practice to handle the task effectively with the non-dominant hand (Fig.2 a,b). The ultrasound transducer should be held in the non-dominant hand, while the dominant hand is used for injection. Full visualization of the entire injection process under ultrasound guidance is not required; once the cannulatip is confirmed to be clear of vascular structures, the transducer can be removed, allowing the injector to continue with both hands.4
To ensure smooth procedure flow, the assistant should be trained in handling the ultrasound equipment, including adjusting the gain, Doppler mode, and repositioning the device as needed. Additionally, they should be prepared to assist in the procedure by providing the injector with necessary materials.
Some injectors prefer to work in partnership with a sonographer. In this setup, one physician performs the injection while the other guides the procedure with the ultrasound. Typically, the sonographer is positioned on the right side of the patient, with the injector ideally on the left. Close coordination between the two professionals is essential to ensure an efficient treatment flow.
Ultrasound-guided filler injection techniques
To enhance clarity and provide guidance on using ultrasound during filler injections, our team has organized the approach into two primary techniques:5
Scan before injecting
This technique involves assessing the treatment area prior to injection to identify and avoid critical structures like arteries, glands (e.g., parotid), and foramina. It is especially valuable when using a needle at a perpendicular angle to the skin, as it can be challenging to position the transducer parallel to the needle, making real-time scanning during the injection impractical. We also use this technique to mark vascular structures on the skin in high-risk areas, such as the glabella, where both techniques may be combined.5
The steps for this technique are as follows:
-
Identify and mark the intended injection point on the skin.
-
Use Doppler ultrasound to scan this point, checking for any underlying structures (e.g., arteries).
-
If no critical structures are detected, remove the transducer and proceed with the injection.
Scan while injecting
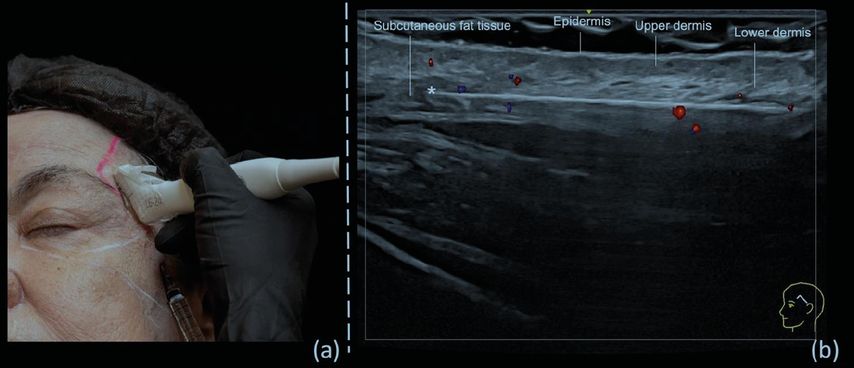
This technique is mainly used with blunt cannulas but can also be applied when injecting with needles inserted at angles other than perpendicular to the skin. In this approach, the cannula is visualized in real time (Fig. 3), allowing precise positioning in the desired anatomical region while avoiding vascular structures.
Fig. 3: a) US guided injection in the temporal region showuing the “scan while injecting” technique in the subdermis; b) color Doppler US imaging showing cannula parallel to the probe and its tip (*) outside of vessels5
Conclusion
The use of ultrasonography as a guide for aesthetic procedures has added safety and effectiveness in the administration of injectables, minimizing complications, particularly those related to vascular structures. Utilizing this technique requires a deep understanding of both anatomy and ultrasound techniques, as well as an understanding of the procedural steps involved. Applying existing protocols for ultrasound-guided aesthetic procedures and developing new guidelines to improve the process is of vital importance for the effective and safe execution of these treatments.
Literature:
1 Lee W et al.: A safe Doppler ultrasound-guided method for nasolabial fold correction with hyaluronic acid filler. Aesthet Surg J 2021; 41(6): NP486-92 2 Lee JG et al.: Facial arterial depth and relationship with the facial musculature layer. Plast Reconstr Surg 2015; 135(2): 437-44 3 Gonzalez C, Wortsman X: How to start on dermatologic ultrasound: basic anatomical concepts, guidelines, technical considerations, and best tips. Semin Ultrasound CT MR 2024; 45(3): 180-91 4 Vasconcelos-Berg R et al.: Doppler ultrasound-guided filler injections: useful tips to integrate ultrasound in daily practice. Aesthet Surg J 2023; 43(7): 773-83 5 Sigrist R et al.: Best practices for the use of high-frequency ultrasound to guide aesthetic filler injections - part 1: upper third of the face. Diagnostics (Basel) 2024; 14(16): 1718
Das könnte Sie auch interessieren:
KI in der Dermatologie
Die Dermatologie zählt zu den Fachgebieten der Medizin, in denen visuelle Befunde eine zentrale Rolle spielen. Die Haut als grösstes Organ des Menschen erlaubt oftmals eine Vorhersage ...
Systemtherapie des HER2-low fortgeschrittenen Mammakarzinoms
HER2-low- und HER2-ultralow-Mammakarzinome stellen besondere Herausforderungen dar, da sie sich sowohl in ihrer Prognose als auch im Therapieansprechen von HER2-positiven und HER2-zero- ...
Die menschliche Haut in der modernen Kunst
Dr. Ralph Ubl, Professor für neuere Kunstgeschichte an der Universität Basel, stellte sich der schwierigen Herausforderung, einem Raum voller erwartungsvoller Dermatologen das Organ Haut ...